Welcome to Part 2.
When Baby Girl and I got up to the PICU I still didn’t know what was wrong with her or what was really happening. They got her into a room and got her comfortable. She was relatively stable now. I would have no idea that we would spend the next 29 days in that room; in retrospect so many of those days blur together.
She was admitted on Friday, February 13th, 2015. I think I am just now making the “Friday the 13th” connection but I’ve digressed. The first hypothesis was that she probably caught a virus during her surgery or subsequential time in recovery. They ran a battery of blood tests and chest and abdominal x-rays. In the mean time she was given higher oxygen support. They thought she was just really constipated from the surgery and the pain medication. They explained that all the back up was putting pressure on her diaphragm making it difficult for her to breathe. That sounded way to simple but they were the doctors: all-knowing godlike medical geniuses. They gave her laxatives and suppositories and we waited for her to, um, clear out her system.
♦
Baby girl was still tiny at this time. She had to be at least 10 pounds for the cleft lip surgery and she had just passed that requirement. A lot of the supplies in the PICU were too big for her so the nurses often had to call up to the NICU for specific items. The first time her nurse called up I told her to tell them it was for “[Baby Squirrel’s first name], she’s on a first name basis in the NICU. She’s kind of a big deal.” Her nurse didn’t get the joke and gave me a dismissive short laugh, like a, “Yeah, right. They see so many babies up there they are not going to know your daughter by just her first name.” But the nurse name dropped her like I said and it worked. The supplies were brought down right away and our old nurses and coordinators came down to see her. They would continue to come visit us for the duration of our stay.
♦
The doctor working the day she was admitted had the weekend off. I knew she was sick but I don’t think it dawned on me just how sick she was until that doctor returned the next week and told me she had actually pulled up Baby Girl’s chart on her days off to make sure she was still here. She didn’t mean if she had gone home… She honestly wasn’t sure if my daughter would have survived the weekend.
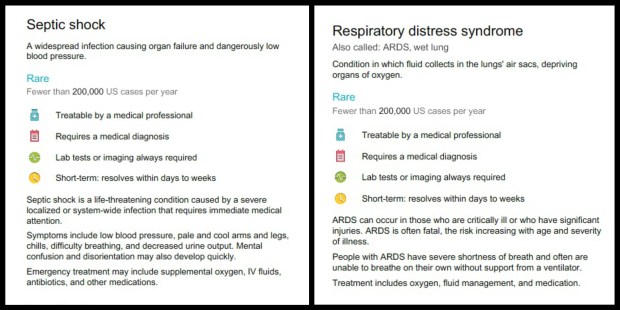
It was finally explained to me that she had been experiencing septic shock when I had brought her in. Septic shock. Our 5 month old, 10.5 pound baby daughter had septic shock. In Baby Girl’s case, the septic shock had trigger Acute Respiratory Distress Syndrome (ARDS).
Septic shock is a serious medical condition that occurs when sepsis, which is a body-wide inflammatory response to infection, leads to dangerously low blood pressure. The primary infection is most commonly by bacteria, but can also be by fungi, viruses, or parasites, and can be located in any part of the body, but most commonly in the lungs, brain, urinary tract, skin, or abdominal organs. It can cause multiple organ dysfunction syndrome (formerly known as multiple organ failure) and death. The mortality rate from septic shock is approximately 25–50%.
–https://en.wikipedia.org/wiki/Septic_shock
[Wiki again, I know, doin’ my bachelor’s degree proud.]
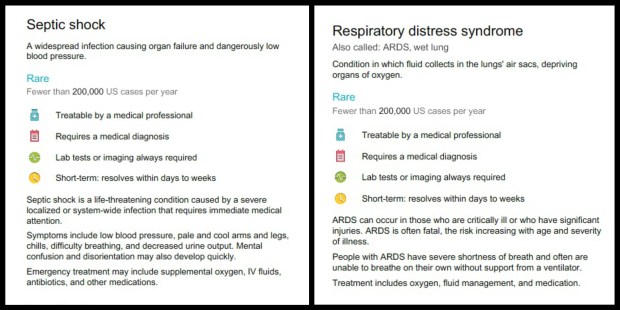

I think you get the point.
However, I still think I was oblivious to the severity of her situation. The intraosseous catheter in her leg was not meant for long term use. They tried again to give her a traditional IV but blew all her available veins and she was becoming dehydrated. They ended up giving her a PICC line, a long term IV more or less, in her left shoulder, and removed the IO from her leg. Like the drill to her leg, it took multiple attempts to place the PICC line. She was getting multiple x-rays a day to view her lungs. Respiratory therapists were working with her around the clock. She couldn’t control her body temperature so a rectal thermometer probe was inserted for constant monitoring. To monitor her urine output they inserted a catheter into her bladder; from our chair/bed we could watch the yellow fluid collect in a vial hung from the side of her crib. She was on such a high flow of oxygen they had to put a strap around her head and under her chin to keep oxygen from escaping out her mouth before she had a chance to inhale it all. But she was awake and responsive most of the time. And that’s kind of how the first week went.

2/15/2015 | Day 3: Strap around her head is to reduce oxygen leakage through her mouth before being inhaled.

2/17/2015 | Day 5: Our view of our daughter from the chair/bed

2/18/2015 | Day 6: Her lip 1 week after surgery (wow!)
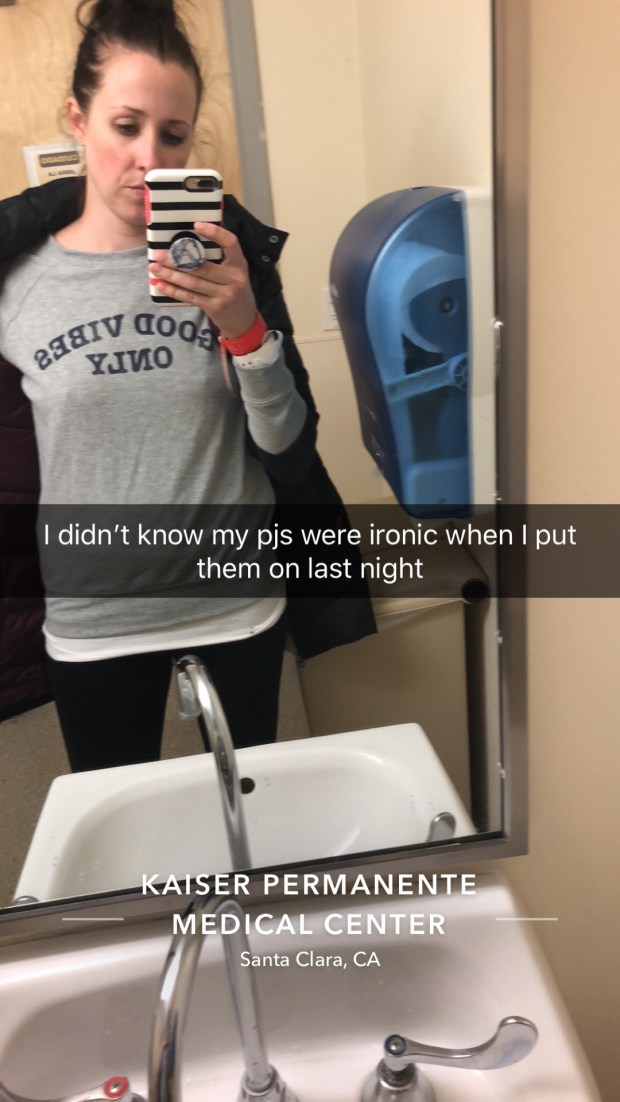
We fell into a routine. My husband would stay with her at night till 6AM when he would leave for work. During the day I would find someone to watch Baby Boy, we didn’t want to risk exposing him to anything at the PICU, so I could be to the hospital before 9AM rounds and stay with her till 3:30PM. She wasn’t stable enough to be held so I spent my days there reading To Kill A Mockingbird and pumping. My husband would get off work at 4PM and head straight to the hospital to repeat the routine. We didn’t see each other at all during the week. So we started leaving funny notes and drawing for each other. One thing I will pat ourselves on the back for is our ability to keep a sense of humor even in the worst of times. Call it our coping mechanism, it’s the glue that holds us together when everything is falling apart, it works for us.

2/19/2015: I haven’t seen my husband in a week

2/20/2015: I haven’t seen my husband in a week

2/20/2015: I haven’t seen my husband in a week
The scariest day of my life, Friday, February 20th, 2015, started normally, well our new normal anyways. My sister came over in the morning to watch my son and I went to the hospital. Baby Girl hadn’t been improving like they had hoped and expected to see after a week. When she was admitted, even with as sick as she was they guestimated she’d be there 10 days. The talk of pneumonia became more frequent but nothing seemed specifically worse. I had to leave a little early that day to pick up my husband’s mother from the airport. She had come to stay with us to help watch Baby Boy. Right when we got home from the airport my husband called me and sounded worried. He said they were talking about intubating her – placing a flexible plastic tube down her throat and through her windpipe to maintain an open airway. I was shocked that things seemed to have escalated so severely since I had left earlier. My husband agreed to keep me updated and call me later.
I left my office and went into the kitchen to update my sister and mother-in-law about what my husband had said. Before I could finished my husband called again.
“Get here now.”
Without questioning, and with a rapid “I gotta go, oh my god, I have to go right now, [sister] tell [MIL] what to do. Bye” I ran out the door.
I rushed to the hospital. I debated whether if a cop lit me up if I would pull over or let him chase me to the hospital. The whole way there with tears streaming down my face I screamed at the top of my lungs at my daughter. I pleaded with her. I threatened her. I begged her. I begged her not to die. At least not till I could get there. I called to any god that if this was the end at least let her go in my arms.
I ran into the hospital from the parking lot. Today for some reason I had diverted from my usual yoga pants and running shoes and was wearing heeled boots. Once inside I ripped them off and ran through the corridors in my socks. People know to get the hell out of your way when they see someone sprinting through the hospital. The elevator to the third floor felt like it was passive-aggressively taking as long as possible. I pressed the PICU doorbell continuously till someone let me in. I hurried to her room on the back wall. My husband was standing outside with a nurse in a red shirt and I could see my daughter’s bed surrounded by the attending doctor, nurses, respiratory therapists, and x-ray technicians, all wearing full length blue plastic gowns, gloves, masks, and hair covers. The light in her room felt blinding.
I demand from the nurse and my husband, “What’s happening?”
When you think your child’s life is on line and there is nothing you can do about it, you want that question answered before you finish asking it. After a one second pause I ask it again. I was a fraction of a millisecond away from screaming, “What the FUCK is happening?!” in the nurses face when she finally opened her mouth and calmly and quietly started to explain. I can’t remember what she said, only that it pissed me off she was being so calm.
When they finished intubating her and sedating her the doctor sat down with us in our room and explained everything to us. Baby Girl had double pneumonia. She was intubated and put on a ventilator and oscillator. This would allow her to stop working so hard to breathe and open her lungs up. However, and this was the hardest part for me, she had to be medically paralyzed. Movement could cause additional injury to her airways. So there our daughter laid, motionless, eyes ajar, looking like a vegetable…
My husband had called my sister and asked her to come to the hospital. He would later tell me it was because he worried if anything happened to our daughter he wouldn’t be able to handle me on his own.
I didn’t take any photos for many days. I hated looking at her. I wanted to beg them to tape her eyes shut. Instead they put thick lubricating drops in them to keep her eyes moist. If things weren’t already bad enough on their own, it was later discovered that when they intubated her they had pushed Staphylococcus bacteria into her lungs causing a staph infection on top of double pneumonia. Here are some pictures and videos because I don’t have the words.

2/21/2015 | Day 9 – notice the brick of med ports next to her running lines from the tower of medication pumps.

2/24/2015 | Day 12: Intubated and paralyzed

2/26/2015 | Day 14

2/26/2015 | Day 14: All we could do while she was paralyzed was change her bows
2/26/2015 | Day 14: All we could do while she was paralyzed was change her bows
For the month we were in the PICU my life was completely bipolar. While at the hospital with my daughter during the day, helpless to do anything but watch her motionless body and hope some numbers somewhere start to improve, at night I was at home with my son watching him learn to stand, and jump, and eat solids. I wanted to live in these moments of just the two of us forever. My favorite thing in the entire world was when he would wake up at 4AM and I would bring him into bed with me to nurse and sleep on top of me till morning. Those are the only moments since they were born that I wish I could go back to.
When I got to the hospital each morning I was angry yet numb to the fact of having to be there. I hated that our life was again back-and-forth from this hospital every single day. It was even worse for my husband. He was either busting his ass at work or at the hospital with our daughter. His body hurt from sleeping on the hard sleeper chair that was much to short for his 6’4″ stature. Every night her alarms and monitors would wake him countless times leaving him perpetually exhausted. However, I think the hardest thing for him was not seeing his son and missing his milestones.

3/2/2015: Baby Boy learning (and loving) to jump

3/5/2015: Baby Boy learning to eat

2/17/2015: Baby Boy learning to stand

3/7/2015: Baby Boy ready to socialize

3/7/2015: Baby Boy after too much tequilla

My favorite kind of moments in the whole world
For nearly a week Baby Girl battled double pneumonia and a staph infection. Her doctors were running out of options and were clearly getting worried. We were essentially holding our breath and just waiting and hoping she would turn the corner. Her doctors scheduled a “Family Meeting” for Thursday, February 26th, 2015 to discuss her situation.
The day before the meeting an amazing thing happened, apparently. She was still intubated and on the ventilator and oscillator but her stats started to improve. And they continued to improve. She had rounded the corner. I was finally feeling assured that my daughter would not die.
I remember standing at the foot of her crib talking to her and playing with her feet when a woman sobbing and screaming entered the PICU and made her way, practically carried by her partner, to the room next to ours. The doors to each patient room are glass but typically a curtain is half pulled for privacy, and unspoken etiquette is you don’t more than glance into another patient’s room. There was a lot of activity, a lot of coming and going from the nurses to the room next to ours. Two chairs were put outside our rooms so the woman could collapse into one of them rather than on the floor. She just kept screaming “No! No!” over and over. Our nurse came and closed our sliding door but it only slightly muffled her cries. Her sobs turned to retches and she threw up on the floor.
Something clearly awful has happened or was happening in the room next to ours. I didn’t see a doctor again for hours. I was able to establish that after the child was brought to the PICU he was quickly rushed into surgery. I was so acutely aware that I was on cloud 9 at the prospect of my child finally improving, while this other mother was in the pits of a hellish nightmare. Selfishly I was so relieved that Baby Girl was seemingly over the worst of it by this time because I think that mother’s cries would have been the final straw on the proverbial camel’s back that was my mental sanity.
The next day was our Family Meeting with Baby Girl’s team. We were led to a small conference room outside of the PICU. The head doctor began the meeting by expressing that he had expected this meeting to have a much different tone before her recent improvement. He had scheduled the meeting originally to discuss preparing ourselves for the end. For the possibility of her not improving after they exhausted their options. Instead we spent the time making a plan for her recovery.
Over the next couple days, while still intubated, they allowed Baby Squirrel to wake up a bit. She would take breaths on her own, establishing that she would be prepared for extubation. It was the most amazing thing to see her look around with her big blue eyes, the eyes I feared for so many days that I would never see again. Her eyes represent so much to me. They were tiny and black, alien-ish, when she was born. They made her look so sick, I hated them. But the more she grew the bigger they grew. And her eyelashes! Her eyes are lined with the most amazing long, perfectly curled lashes. Her eyes became the first thing people notice about her, the only pleasant feature of her face for so long. While still in the NICU, I would stare into her eyes trying to force my will and any energy I could possess of the universe into her to heal her. So when she was able to blink and look at me, and look into my eyes again, my heart erupted with joy.
2/28/2015 | Day 16: Baby Girl is able to wake up and look around, while hoping a nurse wouldn’t notice and sedate her again
When the decision was made that she did not need to be paralyzed anymore I shared this:

2/28/2015 | Day 16: Best day!!!
“This might look scary but to me it’s AMAZING! 3 days ago we weren’t sure if she would survive. Her doctors were clearly worried and running out of options. I thought I would never see my daughter’s big bright eyes again. Thankfully [Baby Squirrel] rounded the corner just in time and is improving everyday. Today they reduced her sedatives enough to allow her to wake up and play for 30 minutes before the nurse caught us and sedated her again. In the last 2 weeks our little fighter has battled septic shock, pneumonia, a viral infections, staph infection, and ARDS. She reminds me everyday that my faith in her is not misplaced. She is my hero.”
At the time I was not as open about my daughter as I clearly am now. I didn’t share much to anything about her on social media. I was and still am extremely hyper-aware of how uncomfortable and scared she makes people around her. I knew this photo would be hard for people to see, and harder to understand that it was actually an amazing moment for our family.
The next day the breathing tube came out and she was placed back on a high-flow cannula. She was still on a lot of opiate painkillers and kept sedated to help her continue to heal. But she wasn’t paralyzed!!!

3/1/2015 | Day 17: Extubated
As we continued to receive more good news each day, we would watch distraught family members visit the child in the room next door. We tried to give them their privacy and not make eye contact when we would pass them in the corridor; however, we would also try to catch a quick glimpse of the child as we passed. When I finally caught a glance his head was completely wrapped in white bandages.
On March 2nd, 2015, after 18 days I was finally able to hold my daughter again. I pulled a chair next to her crib and held her while we slept. She still had her PICC line and med ports which had to be carefully balance around me but she was in my arms. While we sat together I heard alarms and monitors going off in the boys room. Nurses speed walking to and fro. Quick frantic communications. A crash cart was called. The mother was sobbing unconsolably in the hallway, helpless. With pangs of guilt I hugged my daughter tighter.

3/2/2014 | Day 18 – First time holding her since she was admitted

3/2/2015 | Day 18: Lots of opiates in this little girl
And then the kid was gone. I didn’t see them take him away. All evidence of what had happened in that corner room was gone. I could feel the closeness of the morgue 3 floors below. My heart ached for the family knowing the motionless shell of their child was down there. I was overwhelmed by the complete and udder unfairness that children can die. Being a mother exacerbated that feeling. So fucking unfair. In the times since then that Baby Girl has been to the PICU we always hold our breath and pray she’s not put in that corner room. Any room but that room. As if the polarities of our adjacent situations weren’t more apparent, on March 3rd, 2015, the twins turned 6 months old and Baby Squirrel smiled for the first time.

3/3/2015 | Day 19: Baby Squirrel starts smiling for the first time! (mostly at her cute male nurse.)

Baby Boy
Baby Girl continued to improve and was started on methadone to help wean her off the opiate painkillers she had been on for so long. It felt like they were pricking her heel to check her blood-gas every hour, maybe they were. Watching a child withdrawal is so sad. She was sweaty and restless and you could tell by her movement that she was itchy. They gave her Benadryl and other non-opiate sedatives to keep her comfortable. In the meantime we thought we would take advantage of her being sedated and have the audiologist come to her bedside to redo her hearing exam. During her cleft lip surgery, they had also placed tubes in both her ears. The thought being that sometimes children with cleft palates have fluid build-up in their ears making it sound like they are hearing underwater. The tubes would help elevate that impairment.
The audiologist came and performed her test but her results were inconclusive, again. She thought it was most likely due to interference from all the equipment in Baby Girl’s room – it wasn’t the ideal location for an accurate hearing test. She said she didn’t think the results were accurate because Baby Girl had turned and looked at her when she opened her door and entered her room, which had been outside of her line of sight. Our guess was maybe she was deaf in one ear but that she definitely had some hearing because everyone saw how positively she responded when we would turn on her music or she heard her daddy’s voice. Plans were made to do another sedated hearing test once she was discharged and finally determine the condition of her hearing.

3/6/2015 |Day 22: first semi-real bath in over 3 weeks
When we got to the point that Baby Girl was no longer there because she was dangerously ill but rather because she was being weaned off all her medications, we started putting pressure on the doctors to let us take her home. Of course they were extremely reluctant. Not only did they not want to discharge her till she had been weaned off all her medication, but they also wanted to keep her for observations after that. One thing I learned quickly after first meeting my husband is that he is extremely persistent. He went back and forth with the doctors for days basically negotiating her release. The doctor’s final condition was that we get a pulse oximeter before he would discharge her. If you remember, she had been sent home from the NICU with an apnea monitor. A pulse oximeter would show us her heart rate and oxygenation level. Unfortunately, even though we had the Cadillac of medical plans and Baby Girl had Medi-Cal due to her various conditions and time spent in the NICU and PICU, a pulse oximeter would not be covered. Thankfully from our time there we had gotten to personally know some kick ass social workers and they helped us get CCS supplemental insurance and the pulse oximeter was delivered – ours to keep.

3/10/2015 | Day 26
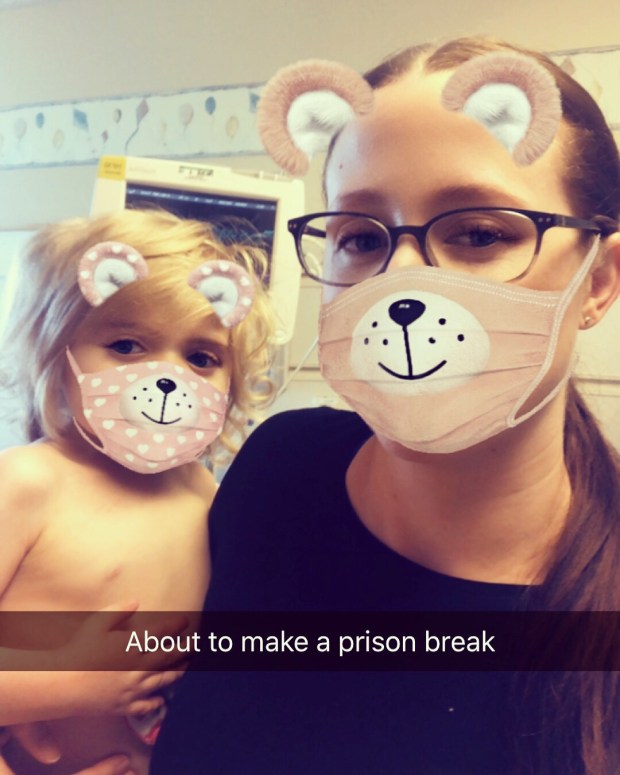
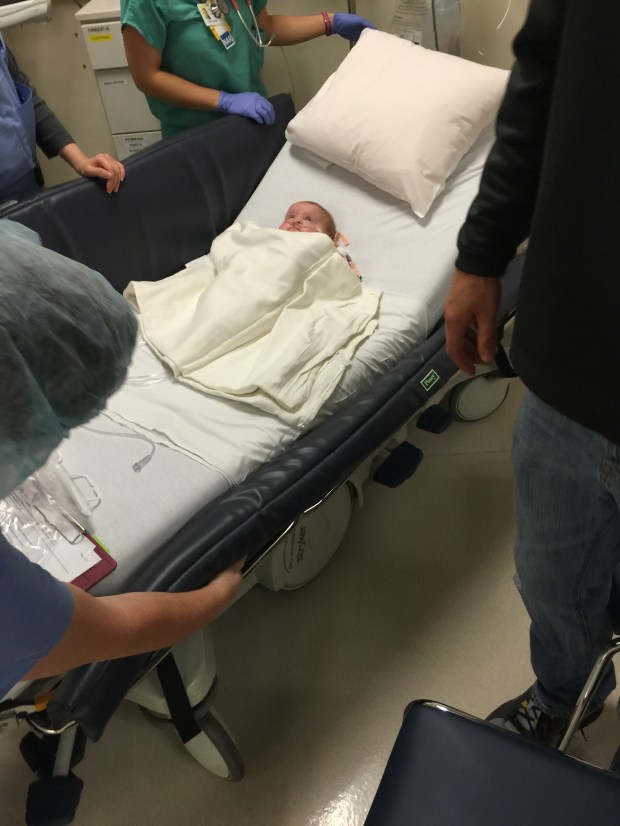
We stayed another week until her medication doses were at a manageable level and on Friday, March 13th, 2015 (another Friday the 13th…) Baby Girl was finally discharged.

3/13/2015 | Day 29: Going home!

3/13/2015 | Day 29: Home at last!

3/13/2015: back in her bed where she belongs
We would have to continue her methadone wean at home since we had convinced the doctors to discharger her earlier than they wanted. When we brought her home she had 16 daily doses of various medications. We were also sent home with a nebulizer and a strict antiasthmatic regimen multiple times a day. We figured it would be easier for us to have her finish her withdrawals and wean at home rather than spend another single night in the hospital. Holy shit were we wrong.
It was such a relief to have her home, to have my husband home. But allow me to say opiate withdrawals are a bitch! The 7PM witching hour returned right on schedule and lasted through the night. If there is one joy any parent of multiples knows too well, is the sick cycle of one waking up and in turn waking the other. Baby Girl was simply miserable. Diarrhea, sweats – nothing we could do to console her. We finally decided to move our son out of our room and into his crib in the nursery for the first time. It made me sad moving him away. For the weeks to come I would try everything at night to help alleviate our daughter’s suffering (and our’s!) But more than once it only resulted in me screaming into a pillow and beating my fists against the bed.
Time passed, she healed, and although she would develop pneumonia about once a month through spring and summer, she spent the next 8 months straight at home, in her own bed every night, where she belongs.
♦
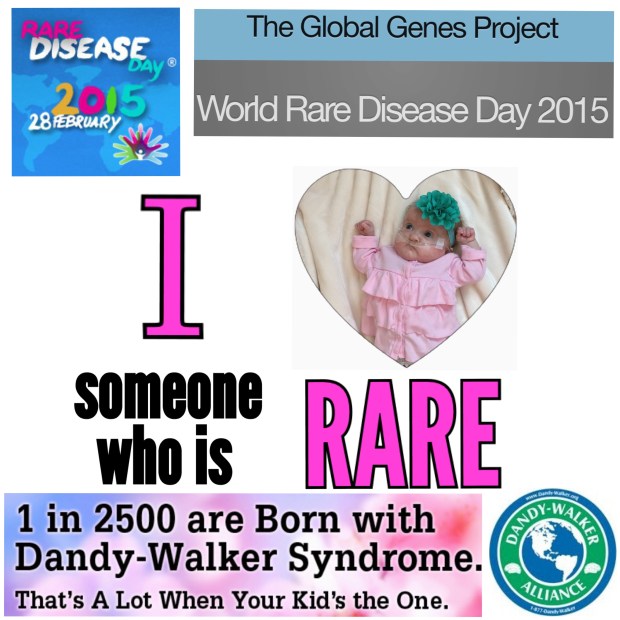
Thinking back we never wanted people to know that there were things wrong with our daughter and didn’t share many photos either. We didn’t want much about her posted on Facebook unless it was something extremely exciting and positive; however, sometimes I would sneak something up on Instagram to share with my close friends. February 28th 2015 was World Rare Disease Day. A couple days before, with nothing else to do while our daughter was paralyzed, I made the collage below but never shared it. It is funny to me now because Dandy-Walker has proven to be the least of her concerns. I will share extensively on this topic of syndromes and genetics in a post to come.