Previously on “Momma Swears A Lot”: Upon learning of Baby Girl’s lack of auditory nerves, genetics got involved again to hopefully find out why they never formed. Since her early birth, doctors have been trying to determine whether her various conditions are due to errors in her DNA, or consequences of prematurity. Prior to the Craniofacial panel meeting, I spoke on the phone with our geneticist. After reviewing Baby Girl’s medical record, the geneticist believed she may have a condition called 3C syndrome. She had blood taken and we waited. Three weeks later the results were back, and like most tests done on Baby Girl, the results were inconclusive:
“The testing we ordered looked at a panel of of 16 genes: AHI1, ARL13B, B9D1, CC2D2A, CEP290, INPP5E, KIAA0196, MKS1, NPHP1, OFD1, RPGRIP1L, TCTN1, TCTN2, TMEM216, TMEM67, TTC21B. The ones most associated with 3C syndrome are KIAA0196 and CC2D2A.
We received the testing result and it was negative – No sequence abnormality was detected. In other words – no spelling error was detected in any of these genes.”
Her geneticist was surprised and the decision was made to do an entire genetic testing of Baby Girl. Four months, and 20,000+ genes later, we had an answer.
♦
Four months prior we entered our geneticists office to discuss what full genetic testing would entail. Along with Baby Girl’s blood, they would also need samples from each of us, her parents. They would not be doing genetic testing on her father and I but rather using our sample for comparison to track the line of inheritance if an error was found in her sample. Like asking a fortune teller how you’re going to die, we signed form after form agreeing to wanting to know whatever the results may be. We also had to decide whether we wanted to know any secondary results that may be found, such as if she carried abnormal BRCA1 or BRCA2 genes, the genes typically thought to be responsible for hereditary breast cancer. This choice also included possible medical and insurance consequences of knowing such information ahead of time. Since the initial seed was planted in my mind that she had suffered a mutation during development the thought of childhood-cancer has also sprung up. We only wanted to do this once, we wanted to know everything.
After an excruciating 4 month wait, and calling multiple times to check on the results, I finally got the call. The call came from the geneticist that had been with us since the beginning, since the ultrasound that initially revealed her cleft lip and palate. They had an answer. She told me that they had found a single mutation that accounted for all her conditions and they wanted us to come in to talk about the findings – in a week and a half… Ten more days of waiting. I made the appointment but I nearly begged her to give me any morsel of information she could.
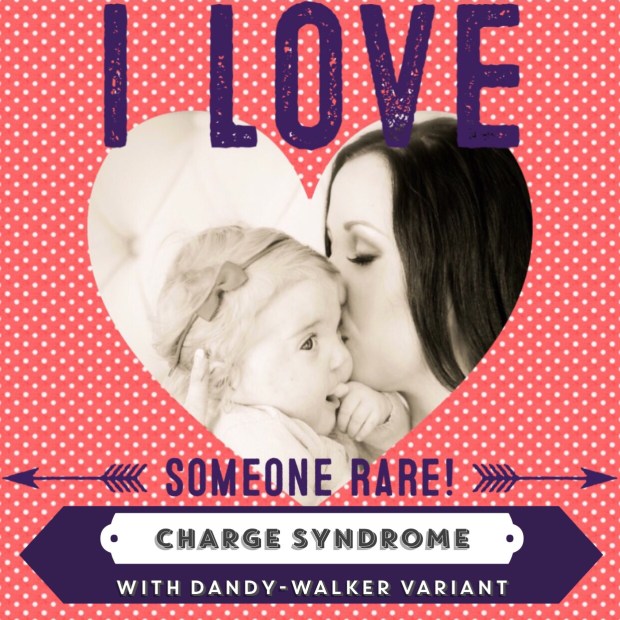
“They found the gene responsibility for a condition called CHARGE Syndrome, like you ‘charge’ your cell phone. As you know I always advise not to search the internet but I know you probably will.”
She went on to tell me one more thing, that the cause of her genetic mutation was “heterozygous/de novo,” meaning it did not come from me or her father but rather was a new, random mutation that likely occurred just after fertilization. In other words, before I even knew I was pregnant. This small piece of information took so much weight off my soul. Not just that we finally had a diagnosis but that I hadn’t done this to my daughter. I had worried that the genetic testing would again come back with no answers and she would end up in the medical books as a new, never before seen case: “Alien Mystery Baby Syndrome.” But more importantly to me was that there was nothing we could have done to cause or prevent this.
After hanging up the phone, I sat back in my dining room chair and stared out the window. I searched for how this diagnosis made me feel. We had desperately wanted answers for so long and they had evaded us at every turn. Now that we had a cause, a condition, with a name, and a prognosis, the pencil sketching of what our future might look like began to look more permanent. Immediately I consciously acknowledged that I would have to let go of the thought that all her conditions were coincidental and she would one day outgrow them and be “normal.”
Initial routine pregnancy testing had said we had a very low chance of having offspring with a genetic disorder. And later when I underwent a double amniocentesis, the chromosomal results for both twins had come back normal. Our geneticist had warned us then that it didn’t rule out genetic disorders, but in our naive minds it did. Since her birth the common consensus was that the remedy for most of her conditions would be time.
“Once she gains weight she’ll be fine.”
“Once she gets a little older and bigger she’ll be fine.”
“Once they send her home she’ll start catching up.”
“By the age of two she’ll be caught up and be a normal kid.”
“When she finally gets past all this stuff she’ll be just like everyone else.”
The geneticist was right, I would Google “charge syndrome”, for hours in fact. I needed to wrap my head around what it meant before I called my husband to give him the news. He had been my rock through everything but I knew he would need me to be his on this one.
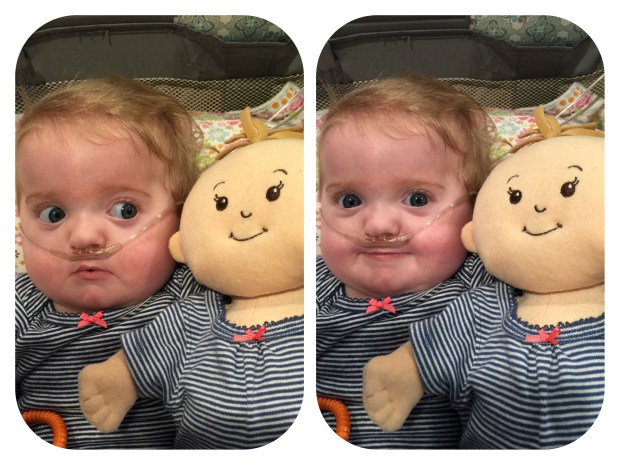
The first thing I saw was the faces of children with CHARGE syndrome. I was terrified looking at their malformed faces. At every turn our geneticist had warned us about looking online because you are likely to find the most severe cases. However, looking from those pictures to my girl, she didn’t look like them. She shared some of the facial features but her’s were softer, less profound. I remember thinking how glad I was that we hadn’t received this diagnosis during pregnancy because these photos would have been even more terrifying. In Baby Girl’s case, she didn’t have every characteristic of CHARGE Syndrome, but CHARGE Syndrome explained all of her unique characteristics.
“CHARGE syndrome is a disorder that affects many areas of the body. CHARGE stands for:
Coloboma of the eye
Heart defect
Atresia choanae (also known as choanal atresia)
Retarded growth and development
Genital abnormality
Ear abnormality
The pattern of malformations varies among individuals with this disorder, and infants often have multiple life-threatening medical conditions.”
–https://ghr.nlm.nih.gov/condition/charge-syndrome
*For additional information I have included a full chart of characteristic, descriptions, frequencies, and links to pictures at the bottom of this post.
The day finally came in late October 2015 to meet with our genetic team and discuss the findings. By then I had visited countless websites, read hours worth of articles, and started to digested her diagnosis.
When our genetic team greeted us I sensed they were trying to be very gentle with us. We showed them that was not necessary. We commented that we must be the only parents to be happy and laughing about the news of their child having a genetic disorder. Of all the countless tests our daughter had endured, this one finally gave us an answer, a solid spot to push off from, a game plan. Not to mention to keep her Medi-Cal coverage we financially needed a diagnosis. They reiterated what they had told me over the phone about her condition and went over the defining characteristics.
Coloboma of the eye: clefting in the eye, she does not have this characteristic. She has since been prescribed glasses for farsightedness, but otherwise her eyes are normal. 80-90% of “CHARGErs” (people with CHARGE Syndrome) have significant vision loss or blindness.
Heart defect: she was born with a threatening VSD which defied the doctors by closing on its own in months rather than in years, as expected. She still has a PSO heart defect – typically this hole closes at birth. She receives bi-annual echocardiograms to monitor her condition. At this time she is stable and is not in need of invasive intervention. Continuous oxygen is required to keep her blood properly oxygenated.
Atresia choanae (also known as choanal atresia): a blockage of the nasal passage(s), usually by abnormal bony or soft tissue. Typically this is discovered at birth as the child is unable to inhale through their nose. She does not have this condition; however, her cleft palate has been left open for the purpose of keeping an enlarged airway.
Retarded growth and development: normal birth weight is typically seen and then followed by inadequate growth. This is most likely due to feeding/swallowing issues in infancy, which is most likely the case with Baby Girl small stature. She is currently proportionate in weight-to-height, and her weight is now good for her age but she is markedly smaller than her twin brother. He outweighs her by 8 pounds and is 5 inches taller. It is likely she will forever be smaller than her peers due to her stunted growth in infancy.
Developmental delays are especially common as CHARGErs typically have low muscle tone (hypotonia), and multiple life threatening condition at birth requiring prolonged hospitalizations. Brain and skeletal anomalies compound these developmental delays.
Genital abnormality: visible abnormalities are more common in males, Baby Girl does not have this characteristic. However, they may experience delays in puberty, or need hormonal therapy to initiate puberty. Kidney anomalies are also common.
Ear abnormality: anomalous ear lobes, cochlear abnormalities, balance problems, hearing loss. Kind of, yes, yes, and yes.
Since the designation of the CHARGE nomenclature, additional common characteristics have been attributed to the syndrome:
– Choanal atresia or stenosis: decreased/absent sense of smell
– Cranial nerve problems: facial palsy, hearing loss, undeveloped auditory nerve(s), swallowing problems, reflux, sinus problems
– Cleft lip and/or palate
– Dental problems
– Behavioral concerns
– Brain anomalies: Dandy-Walker Variant in Baby Girl’s case
– Increased pain threshold: potential superhero
And after the geneticists explained all of that, they gave us the Secondary Findings: None.
♦
As wonderful as finally having an answer was, please don’t underestimate our grief. Learning that our daughter had a genetic disorder and would never be “normal” fucking sucked. It’s terrible to have to ask if your child’s life expectancy will be shortened. (The answer being baring complication due to her existing conditions, her life expectancy is apparently normal.) It’s fucking unfair. It is so unbelievably fucking unfair. One in every 10,000 births – not the jackpot I ever dreamed of winning. If she has children someday the odds are 50% her offspring will have CHARGE Syndrome.
I am not a believer of “Everything Happens For A Reason.” It sucks this happened to our family, it’s fucking unfair, and it hurts everyday. I don’t believe there is a reason for any of it. And please please please please please PLEASE don’t try to point one out to me. There are just no words to mend some injuries.
The diagnosis changed the way I looked at her. At first it felt like a veil of expectations had been lifted. She was free to be whatever she was going to be. At first I looked at her with pity, this poor little broken baby of mine. However I think it made me love her more. It allowed me to understand her better. I still have high expectations for her but when she actually accomplishes them it gives me an unbelievable high for days.
The prognosis for every CHARGEr is different and unforeseeable. The verdict is still out for her cognitive ability. I don’t like to skip ahead but the twins were recently assessed as part of their high-risk status of prematurity – our healthcare provider will closely follow their development till the age of three. Baby Boy scored average across the board, and above average in fine and gross motor skills. Proud mama bear over here! They admit their test does not accommodate for hearing loss, and therefore Baby Girl scored in the low average range – which is encouraging. They expect that as her communication skills improve through acquisition of sign language, as well as fine and gross motor skills/strength, that this score will increase. We will meet with a communication specialist in the near future to better assess her skills. They will be tested again in a year, before their third birthday.
I included this information to stress that my daughter is not “retarded.” Yes, she has a major, complex genetic disorder. Yes, she is extremely medically fragile. Yes, she has developmental delays. No, she can’t hear you. But she is watching, and she is learning, and she is much more intelligent than most people give her credit for. As I have mentioned before, I am hyper-aware of how people explicitly and unconsciously act around her. Most outings make me want to scream because people either won’t look at her, walk in a big circle around her, frown at her, or say something along the lines of “poor baby.” UGH!!!! I know children (and adults for that matter) with special-needs make most people uncomfortable, and my daughters medical conditions can make her especially scary at times, but she’s so fucking awesome too. My mommy wish as she gets older is for more people to be able to see that. Like every child, some days they drive you crazy, push you to the breaking point of your mental and emotional sanity, but at the end of the day you couldn’t imagine loving a tiny human any more than you love them.
I tried to keep the genetic information as laymen as possible. Please know, like most genetic conditions, it is extensively complex and cannot be completely, and fairly, explained in this one article.
♦
This post is dedicated to a tiny family in our lives going through a similar experience. It flipping sucks and it’s not fair. You may feel lonely but you are not alone. We each process this news in our own time. We love you! – G, J, A & A

*Major Features of CHARGE Syndrome (very common in CHARGE and relatively rare in other conditions)
| FEATURE | INCLUDES | FREQUENCY |
| Coloboma of the eye | Coloboma (sort of like a cleft) of the iris, retina, choroid, macula or disc (not the eyelid); microphthalmos (small eye) or anophthalmos (missing eye): CAUSES VISION LOSS Pictures |
80%-90% |
| Choanal atresia or stenosis | The choanae are the passages that go from the back of the nose to the throat. They can be narrow (stenosis) or blocked (atresia). It can be unilateral (one-sided) or bilateral (both sides), bony or membranous.
Unilateral atresia or stenosis can be difficult to diagnose |
50%-60% |
| Cranial nerve abnormality | I – Missing or decreased sense of smell | 90-100% |
| IX/X – Swallowing difficulties, aspiration – Pictures | 70%-90% | |
| VII – Facial palsy (one side or both) – Pictures | 40% | |
| CHARGE outer ear | Short, wide ear with little or no lobe, “snipped off” helix (outer fold), prominent antihelix (inner fold) which is discontinuous with tragus, triangular concha, decreased cartilage (floppy), often stick out, usually asymmetric – Pictures | >50% |
| CHARGE middle ear | Malformed bones of the middle ear (ossicles): CAUSES CONDUCTIVE HEARING LOSS | Common |
| CHARGE inner ear | Malformed cochlea (Mondini defect); small or absent semicircular canals: CAUSE HEARING LOSS AND BALANCE PROBLEMS – Pictures | 90% |
Minor Characteristics of CHARGE: Significant, but more difficult to diagnose or less specific to CHARGE
| FEATURE | INCLUDES | FREQUENCY |
| Heart defects | Can be any type, but many are complex, such as tetralogy of Fallot | 75% |
| Cleft lip +/- cleft palate | Cleft lip with or without cleft palate, cleft palate, submucous cleft palate – Pictures | 20% |
| TE fistula | Esophageal atresia, Trancheo-esophageal fistula (TEF), H-shaped TEF | 15-20% |
| Kidney abnormalities | Small kidney, missing kidney, misplaced kidney, reflux | 40% |
| Genital abnormalities | Males: small penis, undescended testes Females: small labia, small or missing uterus Both: lack of puberty without hormone intervention |
50% 25% 90% |
| Growth deficiency | Growth hormone deficiency | 15% |
| Other short stature | 70% | |
| Typical CHARGE Face | Square face with broad prominent forehead, arched eyebrows, large eyes, occasional ptosis (droopy lids), prominent nasal bridge with square root, thick nostrils, prominent nasal columella (between the nostrils), flat midface, small mouth, occasional small chin, larger chin with age. Facial asymmetry even without facial palsy – Pictures | |
| Palm crease | Hockey-stick palmar crease – Pictures | 50% |
| CHARGE Behavior | Perseverative behavior in younger individuals, obsessive compulsive behavior (OCD) in older individuals | >50% |
Other Features of CHARGE: consistent with CHARGE, possibly medically significant, but less helpful in making a diagnosis
| FEATURE | INCLUDES | FREQUENCY |
| Chronic ear problems | Lots of infections, fluid in the ears, PE tubes until teens | 85% |
| Sloping shoulders | Underdeveloped shoulder muscles, small or missing pectoral muscles, short neck – Pictures | Common |
| Limb/skeletal | Absent thumb, extra fingers, vertebral abnormalities | ? |
| CNS abnormalities | Hydrocephalus, seizures, abnormalities seen on MRI or CT | Occasional |
| Thymus or parathyroid abnormality | Small or missing thymus, decreased immune system | Rare |
| Omphalocele | Omphalocele or umbilical hernia | 15% |
| Nipple anomalies | Extra, missing or misplaced nipples | Occasional |
| Hypotonia | Low muscle tone – Pictures | 90% |
| Scoliosis | Usually due to low muscle tone | Common |

















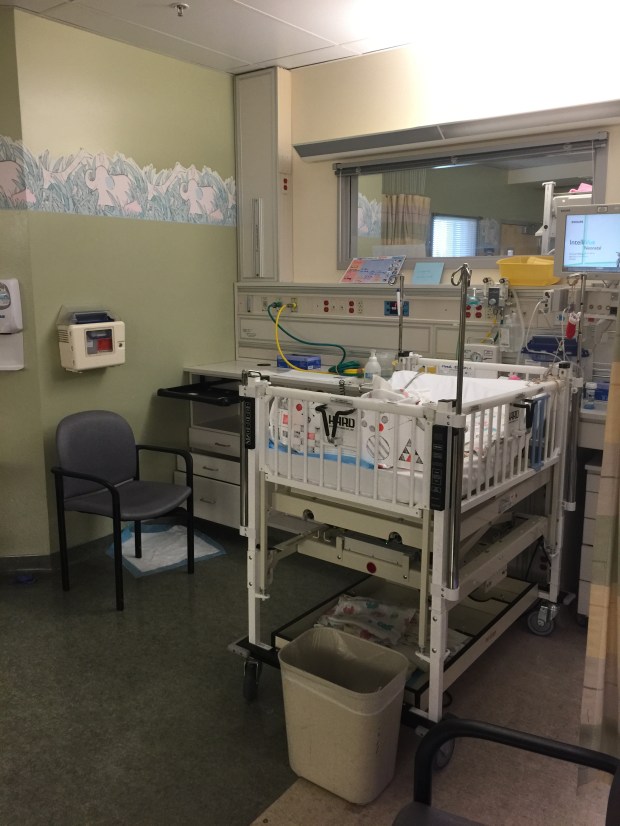
 All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.
All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.