This post may not be for the squeamish or hypersensitive. I have included unpleasant photographs and videos showing post-surgical incisions and extreme medical treatments. This post also includes an outsider’s account of the death of a child. That being said, the story I am going to share was profoundly traumatic for our family, leaving invisible scars that may never heal.
The day Baby Girl came home, January 14th, 2015, was wonderful and terrifying. For 4 1/2 months we had relied on her monitors to tell us exactly what was going on with her, and if something happened the nurses and doctors were right there to intervene. The nurses had told us from day one not to rely on the monitors but to watch her coloring. We quickly learned “dusty” = bad. Nothing is more nerve racking than the moment when those monitors go off and her life, that you have seen first-hand be extremely fragile, is thrust into your hands.

1/14/2015: First night with both babies home
Please notice the copper rod with colorful rubber bands near her head. What you can’t see is her feeding tube hanging from it. We would jury-rig many ways to feed her over the months to come, thankfully they became more sophisticated than this. Probably the hardest thing that we had not been prepared for was the witching hour. Or what you would all call 7:00PM. Every single night at this time Baby Squirrel would start crying and sweating uncontrollably for a solid hour. One of us would have to sit with her and hold and lower her feeding tube as needed. We tried everything to comfort her but eventually, for our own sanity, settled on wearing headphones till the episode passed.
They had sent us home with an apnea monitor, not a pulse oximeter monitor, meaning we couldn’t see exactly what her oxygenation level was or exactly what her heart rate was. Instead it would just beep at us incessantly if her heart rate got too high or too low or she held her breath for more than 15-20 seconds. I don’t think we ever took her monitor off her that first week. Two days after she came home she had doctor appointments, and I remember unloading all her equipment from the car into her stroller and thinking, no baby should require all these cords, people are probably staring. That day we met with her plastic surgeon (yes, my daughter has had a plastic surgeon since before she was born, NBD) and he cleared her for the surgery we had been waiting for for nearly 8 months, since I was 4 months pregnant, the surgery to repair her cleft lip and nose. (Insert Clueless quote here.) She had been the first baby in her NICU to have a special tape placed across her cleft. (The name of the tape is alluding me now as I celebratorily spiked it into the trashcan when she no longer needed it.) Starting shortly after she was born the special tape was placed on one cheek and stretched across and adhered to her other cheek. The purpose of this tape was to pull her gums together, closing the large opening in her gums due to her cleft palate, and to stretch the lip skin so there would not be excess tension on the incision once her cleft lip was repaired.
Five days later we were back to meet with her anesthesiologist for the surgery and an Ears, Nose, and Throat specialist to discuss placing tubes in her ears during the same surgery. I will explain later the reason for the tubes. While we were in the waiting room waiting for this appointment, Baby Squirrel had a giant blow out! (That’s a poop explosion for any non-parents.) She hated being dirty so she was losing her mind. Her monitor starts shrieking out in the quiet waiting room because her heart rate was over 220! Thats really high, especially for something like a dirty diaper. For the next few weeks, and year really, we would spend an average of 3 whole days a week at the hospital seeing her various specialists (pulmonologist, gastrointestinologist, physical therapist, occupational therapist, ENT, neurology, though ironically rarely her pediatrician because her care was so complex.)
When we were home we tried to make up for missed time. There was already a significant developmental gap between the twins but we tried to put them together as much as possible. From spending more than 4 months on her back in a bed her head had become asymmetrically flattened on one side, but most discouraging was she hated to be held. She would throw such a fit she would have respiratory distress if you tried to hold or cuddle with her. I worried perhaps she was autistic but through speaking with other long term NICU parents, I established it’s fairly common among infants that begin their lives not healthy enough to be held. Even at home, her dislike for being held, plus her great need for growth and therefore strict feeding schedule, had her propped up in her crib for many hours of the day yet again.
As you can probably imagine, it was nearly impossible to bond with her under these circumstances. Since they were born we dreamed of bringing them both home and bonding as a family. However, when Baby Girl came home she became more of my patient than my daughter. Not only did she not like to be held, but due to her cleft lip she was never able to breastfeed. So my daughter and I never got to have that magical skin-to-skin breastfeeding induced oxytocin love fest. At nearly 5 months she still didn’t smile so there was no positive feedback. I loved her in the sense that she was my daughter and my flesh and blood, and when bad things happened to her my heart would physically ache, but it came no where close to the love I felt in my bones for her brother. Judge if you must, I don’t like to admit that. It left me feeling extremely guilty and unfair.
Before either of my children were discharged from the NICU hearing and vision tests were performed as prematurity can greatly effect both areas. Both of their visions were fine, however Baby Girl’s hearing test continually came back inconclusive, “Refer” to be specific. We weren’t too concerned because we knew she loved her music and always responded to her daddy’s voice. Upon her discharge from the NICU she was referred to an audiologist to have her hearing rechecked. This appointment did not go well as it required me to hold her, and hold her still – it wasn’t happening. The audiologists did not believe the results were accurate so we rescheduled our appointment to repeat the test and if it still was inconclusive a sedated test was an option.
A week later was Baby Girl’s cleft lip repair surgery.
♦
Before I start writing any of my blog posts I do research. I go through all the photos and videos on my phone from the target time and read through anything I may have written in my calendar or elsewhere. As I mentioned in the beginning, this time period was particularly traumatic, and this is apparent to me because a lot of the photos and videos I have little to no memory of. In addition, many days I have no documentation to refresh my memory at all during this time because there were days I could barely bring myself to look at my daughter.
♦
Tuesday, February 10th, 2015, at 6:30am we arrived at the hospital and Baby Girl was admitted for surgery. We were able to go back with her to get her changed into a gown and wait for the surgeon to come speak with us. We laid the twins together and they fell asleep. Still to this day she is calmed by his presence.
When the time came I took one last photo of her being wheeled to surgery because there was a little voice in the back of my head wondering if this would be the last time I’d see her alive. All surgeries come with the possibility of complications, no matter how routine, plus I am a mother, the mortality of my children is never far from my mind.
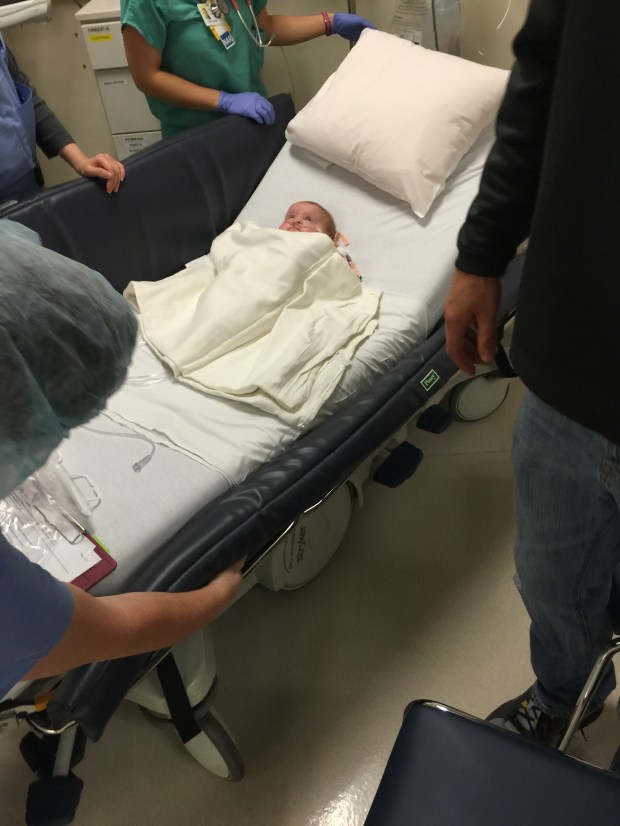
2/10/2015 – Baby Girl being wheeled away for surgery
I can’t recall exactly how long her surgery took but it was quite a few hours. Eventually the plastic surgeon came out and reassured us that everything had gone smoothly and he was really happy with the outcome. We were then directed to Recovery where we would be reunited with our daughter.
Saddest lil’ face you’d ever saw, right?!
But it was also the most amazing! The surgery had completely reshaped her face.

2/10/2015: Her amazing Before and After
Once she was cleared from Recovery we were transferred to the PICU. This was our first time stepping through the big mysterious metal doors. We arrived with our daughter the first time but anytime we had to reenter we had to ring a door bell and announce to the nurse behind the camera who we were and who we were visiting. I was first struck by how much smaller it was than the NICU. There was a centralized nurses/Doctor station on the right surrounded by 7 private rooms with sliding glass doors on the left and back.
She was in a lot of pain but plastics came to check on her and reassured us again that the surgery went perfectly and she was given Hydrocodone/Hycet for pain. As our luck would have it the local hockey team the San Jose Sharks were visiting all the children in the pediatric wing that day, something they do often.

2/10/2015: The San Jose Sharks visit all the children in the Pediatric wing
By that night the doctors felt she was recovering well and transferred her out of the PICU and out to the Pediatric floor. In the PICU the nurses have 1-2 patients. In general Pediatrics the nurses have…I have no idea because we rarely saw a nurse after her move. So of course that’s when the fun started. Baby Girl started screaming and crying and didn’t stop. Her ear-splitting monitors wouldn’t stop going off as her heart rate remained over 220. When the nurse would come to check on her there was nothing they could do for her unless it was time for more pain medication. We resolved to taking turns pacing the halls as a mental health break. Eventually I took Baby Boy home for the night and my husband stayed with her. I would return in the morning to bring her home.
When I arrived in the morning Baby Girl looked like hell and her coloring didn’t look right.

2/11/2015 – waiting for discharge papers, she didn’t look right to me
My husband had left for work by the time I got there but mentioned the crying had lasted all night. As her discharge paperwork was being compiled, her nurse and I simultaneously noticed her MIC-KEY button had come out! The balloon filled with water that holds it in place had ruptured. The feeding tube was still pretty new to me, I had never had to change one on my own. Down the line I would become a super badass g-tube changing pro, but till then I panicked. I knew this commonly happens but I also knew that if the stoma (the hole in the skin through which the MIC-KEY button enters the stomach) were to close she would require another surgery to replace it. We were able to put it back through the stoma and tape it in place until I could get my brother-in-law to go by my house and bring us a replacement button. Hours later I finally had my crying miserable baby home.
For the rest of the day she cried and cried and cried. Then magically the next day she seemed OK. She stopped crying and showed interest in her toys and playing. It was a good day. We still had to keep the arm restraints on her so she wouldn’t touch her lip or nose. Unfortunately, this was just the calm before the storm.

2/12/2015 – Arm restraints so she wouldn’t touch her lip and nose. This was actually a good day, she had energy to play and seemed to be feeling better
That night the witching hour struck and struck hard. Except it wasn’t just an hour, it lasted all night. We kept calling the surgical department and advice nurses and they kept telling us what she was experiencing was normal after a surgery like hers and to continue with the pain medication. She had only been home for 3 weeks before her surgery so we were still learning her but I had a strong feeling something really wasn’t OK. We didn’t have a pulse oximeter and strangely enough they hadn’t taught us how to listen to her lungs. That’s right, our child had chronic lung disease and pulmonary hypertension and we had not been taught how to listen to her lungs, we didn’t even have a stethoscope at the time. At that time we were completely unprepared for recognizing respiratory distress. Paired with the advice nurses telling us that this was normal.
By 3:00AM my husband and I were at our wits end. Baby Girl was clammy, had a mild fever of 101, eyes rolling around in her head – not a pretty sight. At the time her oxygen prescription was 1/8 of a liter of 100% oxygen. That’s barely anything. But with our inexperience, and lack of a proper monitor, we didn’t know if she needed more. We called the advise nurse again and said straight up, “something isn’t right, this isn’t just pain.” We were given an appointment with her pediatrician first thing that morning.
For the ride there I turned her oxygen up to 1/4 liter, still not much but double her usual requirements. She actually appeared more peaceful on the ride but was still lethargic and clammy. While the nurse was taking her vitals like temperature and oxygenation level, under the florescent light of the pediatric clinic she looked extremely pale. Her oxygenation level was 75%…because she has pulmonary hypertension her oxygenation level really shouldn’t be below 95% for any extended period of time.
Once the nurse put us in our room I honestly think she went and grabbed the pediatrician away from another patient because she came in only a moment later. She took one look at her and in her best calm doctor voice, the one they use when you know they are actually really concerned, she asked, “how high does the oxygen flow go on her tank?” “Four,” I replied. “Go ahead and turn her up to four.” She asked me more questions and before I knew it she was asking a nurse to bring in a wheelchair STAT. (“STAT” is never good. “STAT” was used when the ultrasound found Baby Girl’s heart rate was under 80 leading to their emergent birth. I don’t like “STAT”.) It literally happened so fast. A wheelchair was brought in, they threw me in the wheelchair, Baby Squirrel in my arms, and that nurse RAN me across the campus to the Emergency Department where they had a room waiting in the super emergency section. The rooms they leave empty unless their use is truly warranted. (The toothless nipple-popping presumed crack whore complaining about all-encompassing pain while continually asking for more food, whom which we would see on a future ER visit would not get one of these rooms.) A flood of nurses, doctors, and specialists followed.
While they began looking her over and trying to find veins to start an IV, I tried to reach my husband and tell him to get there. He was over the hill golfing (please don’t judge the guy, he thought, like the advice nurses, that she was just in pain from surgery and it would subside over time.) I can’t remember if I reached him right away or if we played phone tag, my adrenaline was seriously pumping at this time. Thanks to good ol’ Zoloft I had my head together though. I wasn’t crying and I was able to converse with the doctors and answer their questions, all using that calm facade voice. Baby Girl had tiny veins and had always been a hard stick. I hated to see them pin her down while they fished for veins but it wasn’t the first time.
A coordinator called me out into the hallway to sign standard forms while they continued trying to get an IV started. While trying to call my husband again I saw a nurse with what looked like a power drill and thought in the back of my mind that that was odd but nothing more. As I was putting my phone back in my back pocket a nurse came up behind me and grabbed my shoulders softly and told me that they were going to drill into my daughters leg bones to try to start an IV that way. What the serious fuck?! At that instant I saw through the open glass sliding door the drill touch down on her right leg. I turned away and collapsed to the floor. I exploded into wails with my head on my knees and my fingers clasped behind my head. The nurses scooped me up and sat me in a chair. I would later find out the IO wasn’t successful the first time and they had to try again on her other leg.
I don’t remember much after that.
Baby Girl and I were moved back up to the PICU.
My husband arrived 20 minutes later from 30 minutes away.
To be continued…



















