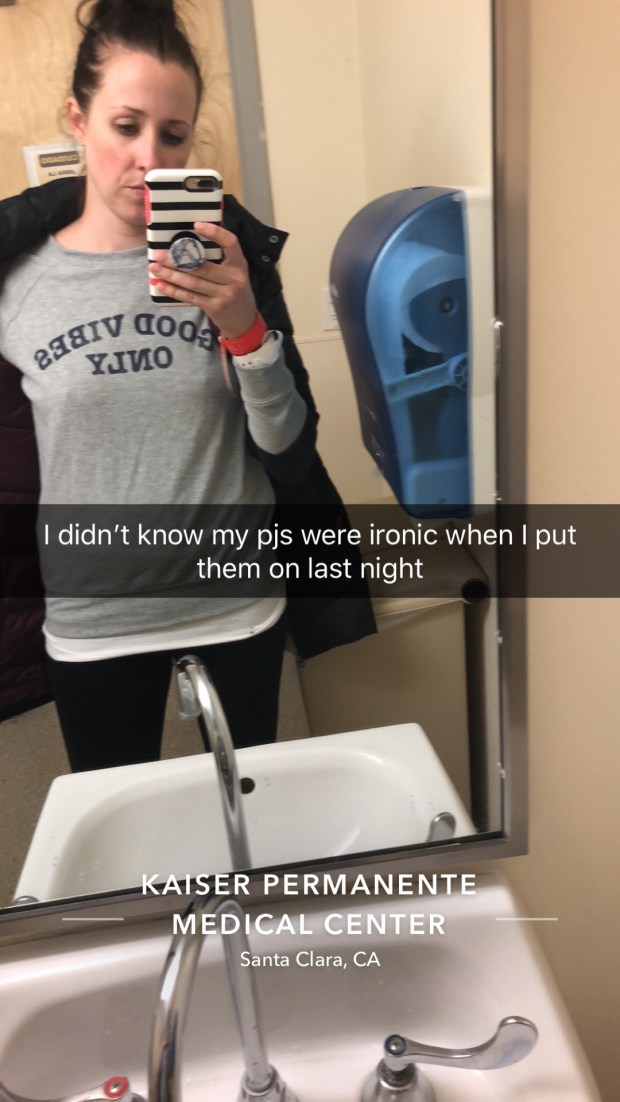
November 19th, 2018: Just seeing the photos from one year ago come up on my Timehop app makes my heart race and fight or flight kick in. Hello Trauma, my old friend. (Bonus points if you sang that outloud.)
♦♦♦
Addie hates Thanksgiving.
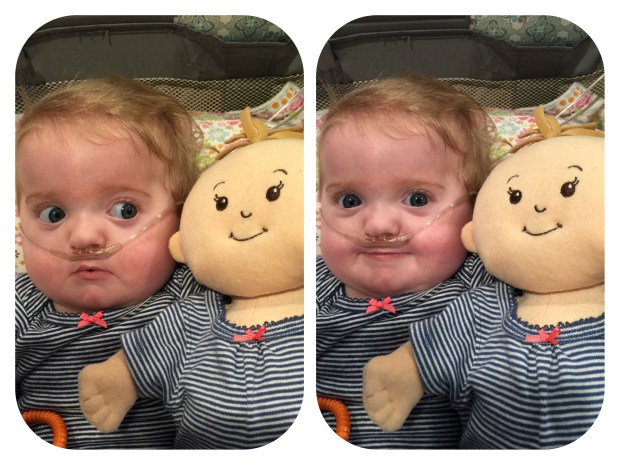
Of the three prior to Thanksgiving 2017, she’d only been out of the hospital and healthy enough to attend one! She’d worn a size 6m onesie as a two year old that said “My First Thanksgiving.” So naturally on November 19th, 2017, just 4 days before we were to host about 20 people at our house, Addie spiked a high fever.
It started low grade for the first 12 hours: 101.3, 99.8, 102.8, 102.5. Since her cardiac catheterization three weeks earlier, where she was started on a daily aspirin regimen to prevent blood clots from forming on the devices patching the holes in her heart, we could only give her Tylenol to manage her fever. Normally I would have alternated giving her Motrin and Tylenol to stay on top of it. Throughout the day she remained playful but seemed a little more tired than her usual self.

I stayed up with her till 12:30am at which point her fever was 102.6 and I was able to give her another dose of Tylenol. I then carried her upstairs to her bed where she woke up and began crying as though she was truly miserable. I sat next to her crib and held her hand, and tried to keep a cool washcloth on her. By 1:30am her fever was up to 103.5 but I still couldn’t give her more Tylenol yet. I continued to sit next to her crib but by 3am I could no longer keep my eyes open and she had settled into a more restful sleep. I checked her temperature one more time, 99.9 *phew!*, and set an alarm for when I could give her another dose of Tylenol.
My husband wakes me up when my alarm starts going off and I get up. I look in Addie’s crib and she looks awful and is burning up again. I check her temperature – 105.1! I wake up my husband and ask him what he thinks I should do since he had been trained as a paramedic in his early 20’s. As he’s getting up to look at her, Addie gasps, contorts, and starts convulsing. She drains of all color, her lips turn blue and foam forms from her mouth. I’ve seen my daughter go through terrible things before, I’ve even had to help hold her down while terrible things have been done to her. This was truly the most terrifying moment because I had zero idea what to do. My husband was so calm and in control while I was completely losing it. And for the first time for either of my children I called 911.

11/20/2017 4:34am
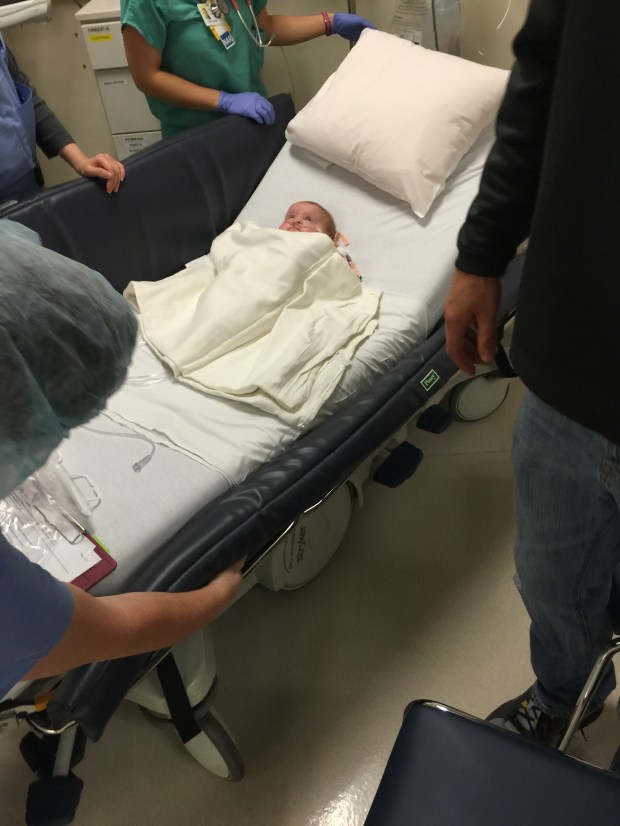
If the notion of me taking this photo concerns you, I agree. I felt dirty taking it. But I took it, as well as all the other “hard” photos I’ve shared on this blog, for the purpose of being able to look back and see all she’s overcome.
It was my first ride in an ambulance and Addie’s second, her first being her trip to Oakland at just a couple months old.
We arrived at the Emergency Department and were greeted by a team ready to take her in. Due to her age and medical history they took her right into room #1. I don’t know how other ED’s work, but at ours the lower the number the more severe they consider you. This room was also the same room where they had to drill into her leg bones to get a line when she had septic shock at 6 months old. Assessments were done, IV was placed, labs were sent, more Tylenol was pushed. At 8am her fever was back up to 103.5. Tylenol could barely touch it. Her labs came back positive for influenza, despite the fact no one else in the house had been sick and we had all gotten the flu shot.
At some point I got up to wash my hands and the nurse says, “oh, there she goes again.” I turned around to see Addie convulsing again. Drained of color again. Lips blue again. Foaming at the mouth again. I helped the nurse try to keep Addie’s body on its side while the seizure ran its course.
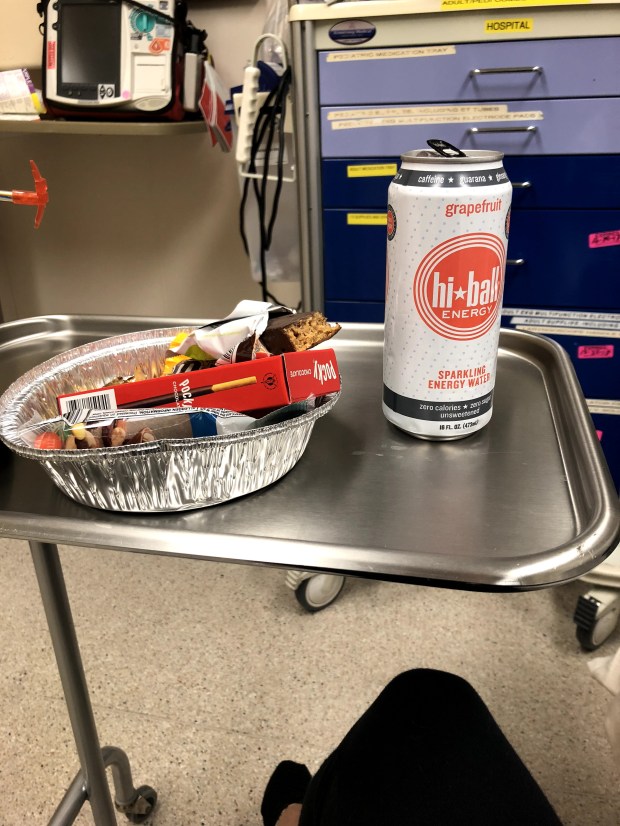
By then I had been awake for nearly 24 hours, excluding the hour I had slept before her initial seizure. The ER doctor brought me an energy water and snacks. She would later email me the following day to thank me for being the most collected and helpful mother of a small child she’d encountered in the ER. *humble brag* (Useless fun fact: Since this day I am still obsessed with grapefruit Hi-Ball and drink one almost everyday.)
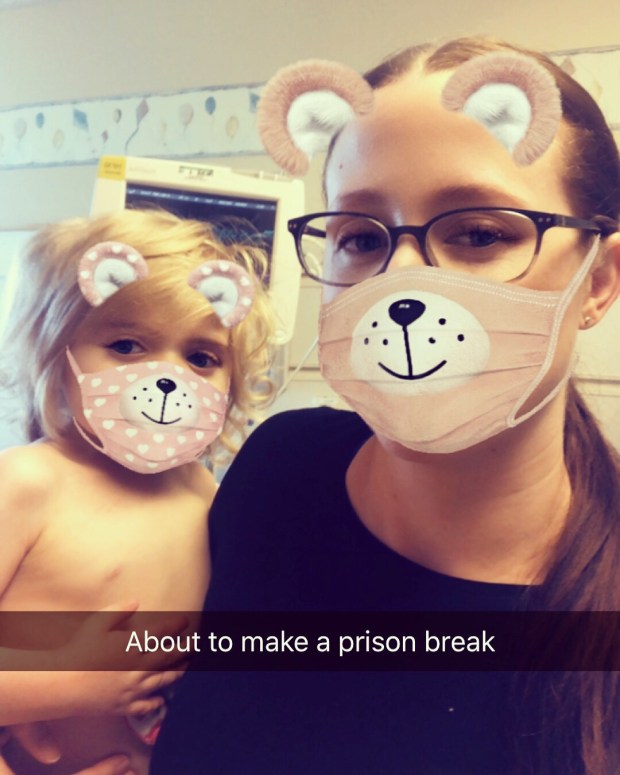
11/20/17 5:31am
After the second seizure the decision was made to admit Addie to pediatrics. It is common for children with high temperatures to have what is called a febrile seizure, however more than one is rare. Given Addie’s complex medical history the doctors had additional concerns and paged her neurologist. In the meantime we were wheeled upstairs to the pediatric department and settled into a private room. Shout-out to our private bathroom, a luxury not supplied in the NICU or PICU.

Making sure she doesn’t fall off the bed.
I tried to curl up at the foot of Addie’s bed to sleep but to no avail. There were only short rails on the bed so I had to keep a hand on her to be alerted if she moved or rolled towards a side. Nurses, doctors, and other staff kept coming in to check her and speak with me. By 11am she seemed to be on the mends. Her fever was back down to 99.1 and she was resting. However, at 11:30am Addie began seizing for a third time. I was alone with her this time. I pressed her call button to get her nurse but it felt like it took forever. When she came it was over but I reported it lasted 30 seconds. In reality it could have only been 10-15 seconds. Time is near impossible to correctly track while in a panic.

Applying cooling measures
Each seizure left her exhausted. Once finished it would take her a moment or so to focus her eyes again and become alert. Her third seizure increased her doctors’ concerns because more than one febrile seizure is uncommon, and that it was while her temperature was less than 100. Her neurologist stated that he wanted her, once healthy, to have an EEG to “see if anything has awoken in her brain.” [WTF mate?! What a chill thing to say, amiright?!]
An EEG is a test that detects abnormalities in your brain waves, or in the electrical activity of your brain. During the procedure, electrodes consisting of small metal discs with thin wires are pasted onto your scalp. The electrodes detect tiny electrical charges that result from the activity of your brain cells.
We couldn’t know it but her third seizure would be her last. Her requirement for discharge became 24 hours without a fever a.k.a. we were spending the night. I told my amazing mom group what was happening and like always they came to our rescue. They sent or delivered food and entertainment to pass the time. Bless them. Their support never ceases to amaze us.
After 36 hours awake Addie’s ex-teacher of the deaf came to visit. I’m nearly certain my eyes were rolling back in my head for her entire visit but I was so happy she came. Addie even showed some love by signing for the lights to be turned off so her light-up Lightning McQueen could shine brighter.
As with our previous hospitalizations, my husband came to spend the night with Addie while my brother and brother-in-law came to drive me and my car home for public safety.
While Addie had still been in the ER, I called and left a message at her daycare letting them know the situation and that she would not be attending that day, or following days. After I went home for the evening our favorite nurses from Addie’s daycare came to visit with toys for Addie and comfy socks and blankets for us. I cried when I later saw what they had gone out of their way to bring us to make our time more pleasant. (Random side-note: I’m rocking the lumberjack socks right now, a year later. Socks are a gift that keep on giving. *wink wink* Honestly, I have a sock problem.)
With all our previous hospitalizations Addie had been in a big pediatric crib. I loved that she was in a regular bed this time so I could lay with her. I had been so tired but I didn’t want to pass up being able to lay with my baby. My husband loved it too but had to request they bring her a crib so he could actually sleep that night.
waiting for the 24 hour fever free mark

11/21/2017: We’re out of here!
Another condition for going home was Addison was started on Keppra, an antiepileptic medication. Keppra comes with a lot of undesirable side effects (sleepiness/ weakness/ dizziness/ zombiness) but since she had had three seizures they didn’t want to wait and see if she would have more. She would go home taking it until her EEG to determine if she truly needed it.
One of her first doses of Keppra at home resulted in her bending forward while sitting indian-style on the kitchen floor and falling asleep in a puddle of her own drool.
♦♦♦
December 7th, 2017: EEG Time!
This was my first experience of any kind with an EEG. They had me wake her up ridiculously early that morning so she would hopefully take a nap during the procedure. The room had a standard hospital bed and the technician asked me to lay down on it with Addie and cuddle her till she fell asleep. HA! Yeah right, Addie is not going to sleep with me, or any one else for that matter, touching her. But we tried. And nothing is more calming to a toddler than putting goo, electrodes, and cotton balls all over their head then topping it with a tight cap. Zen AF.
Needless to say an hour later she was still awake and active. They had already done the strobing light test which thankfully gave neither of us a seizure. But for the rest of the tests she would need to be asleep. I was so worried the tech was going to scrap the test and make us come back another day that I was thankful when she went with my suggestion to put Addie back in her stroller since I knew she was more likely to fall asleep there than in bed with me.
I stayed in the bed, the tech turned off all the over head lights and we waited. She waited, I fell asleep. Best appointment ever. I got to sleep for over an hour! And Addie even fell asleep too. When I woke up I was sure something was wrong because we had been there almost 3 hours at this point. A doctor came in to look at the readings and her and the tech whispered back and forth. Every bad thought was going through my head. Epilepsy, tumors, other terrible possibilities I don’t know about. I don’t even think they can detect brain cancers with EEGs but that didn’t matter to my brain in the moment.
When the tech finally got everything she needed she removed the gunk and electrodes from Addies hair and we were sent home to wait for our neurologist to contact us with the results.
*drumroll*
Results: Normal. Stop Keppra. Rejoice much.
♦♦♦
In 2 days, November 21st, 2018 will mark one year since Addison was last hospitalized.
An entire year.
Our longest stretch of time.
Nobody jinx this.
I’ll find you.
♦♦♦
This will be HOPEFULLY my last depressing post for at least a while. My next will be an update on all the nonshitty things we’ve been up to! A lot of nonshitty things have happened! Stay tuned.