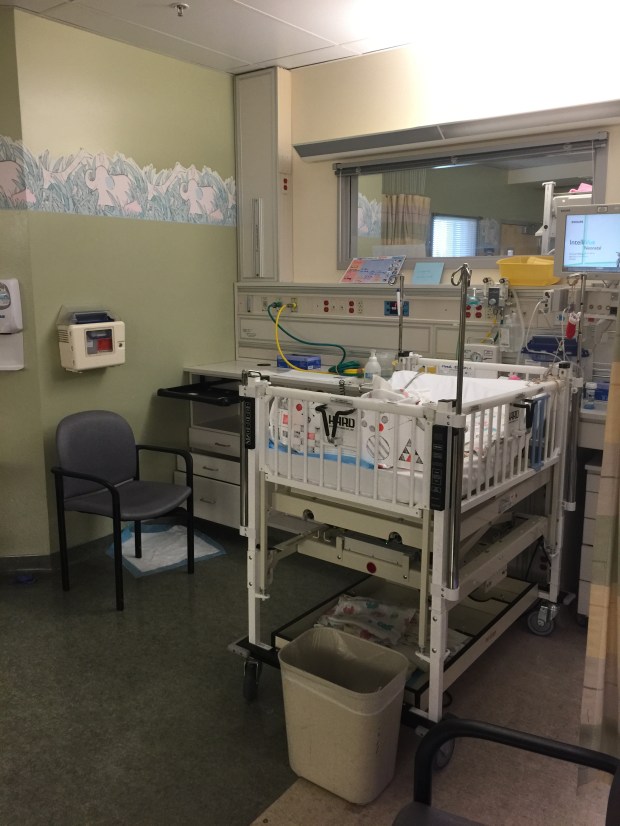
A month after Baby Squirrel was discharge from the PICU after nearly succumbing to septic shock and double pneumonia, we were back at the hospital for a sedated hearing test. The goal being to keep her completely still so we could finally get reliable results.
I was rather optimistic. We figured she had some hearing loss but we knew she could hear. I told her primary NICU nurse that there was a chance Baby Girl was Deaf and she reaffirmed that she was not Deaf, that she loved her music in the NICU and always responded to her daddy’s voice. Even the audiologist that attempted to check her hearing while she was sedated in the PICU believed she could hear because Baby Girl turned towards her when she entered her room out of her line of sight.
My best evidence for her hearing was at home one night when I was putting her to bed, my husband, who was downstairs, spoke through the baby monitor and Baby Girl started looking behind her for him. Yet there were other times when she was napping in the living room and I dropped a pan loudly on the ground and she did not stir. Evidence for her lack of hearing I chopped up to her being used to so many loud noises from her long stay in the NICU.
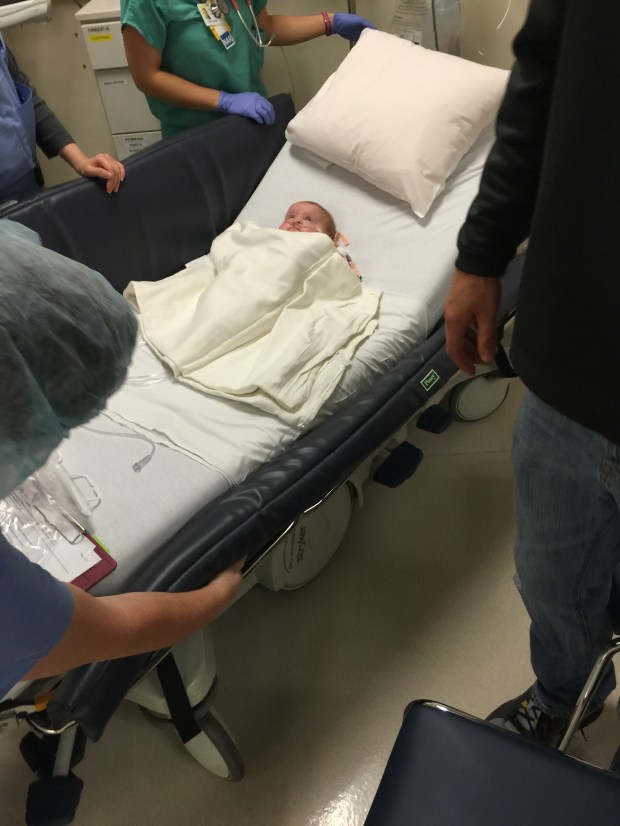
Baby Squirrel’s procedure took place in the same department as my D & C had a year and a half prior. Everyone commented on her being the littlest patient they had in quite a while. Even the smallest infant size gown they had hung off of her. In the photo below you’ll notice she was off oxygen. Around this time she was able to come off often and use it only at night while she slept. Now a year later, this nearly never happens. She’s much bigger now and with the increase in size comes an increase in our hopes that she would be outgrowing her lung disease. If she comes off oxygen now, even for a few minutes, the oxygen in her blood desaturates and she struggles to breathe and turns mottled and blueish. At the current age of 1 1/2, they now expect her to need oxygen till the age of three. *sigh*

When the time came, we went into the procedure room and I sat with her while the nurse tried to start an IV. The attending physician was one of Baby Girl’s PICU doctors (now I jokingly call him “Uncle Ben”). When the doctor and the audiologist were ready I was sent back out to the waiting room to, ya know, wait.
The test took about an hour and then I was brought back into her room for the results. Baby Squirrel’s hearing loss was “Profound.” Meaning she can’t hear. Anything. They tested both ears up to 120 decibels, equivalent to a jet taking off – painfully loud for a person of “normal” hearing. Nothing. The test rendered no response. My heart sank a little but I remember not being surprised. The audiologist said she may have some success with hearing aids, and if we wanted additional testing, an MRI could tell us if she is a candidate for cochlear implants. Before the audiologist left she told me to keep talking and singing to her.
“A cochlear implant is a small, complex electronic device that can help to provide a sense of sound to a person who is profoundly deaf or severely hard-of-hearing. The implant consists of an external portion that sits behind the ear and a second portion that is surgically placed under the skin.”
-National Institute on Deafness and Other Communication Disorders

How cochlear implants work
Typically, to avoid major speech and language delays in a child with hearing loss, it needs to be identified and hearing aids need to be in place by six months of age. Baby Squirrel was now over 7 months old.
A few weeks later I took her to get fitted for hearing aids. She absolutely hated the forming putty being injected into her ear, she screamed and thrashed. This audiologist was so patient and kind, considering both twins were screaming their heads off. I ordered Baby Squirrel hot pink hearing aids – if you can’t hide it, rock it! As we waited for her hearing aids to be made, we moved forward with having an MRI of Baby Girl’s brain. The MRI would look for the presence of her auditory nerves. It was scheduled for my 30th birthday. I prepared for the best birthday present, or the worst.

After MRI and a lot of attempted IVs

Baby Boy had lots of kisses for his sister when we got home
The MRI went smoothly. Our favorite doctor from the PICU, Dr. F, was the attending physician. After, when I was allowed to go back and see my daughter, she was happy and smiley, obviously still enjoying the sedatives. She was covered in tape and gauze where they had attempted multiple IVs since her veins were still so small. Unfortunately, I would have to wait for the ENT specialist to review the images before I would be informed of the results. I emailed her to make sure she saw that the MRI images were ready for her, and sat back and waited to hear from her.
Nothing that day.
Nothing that night.
Nothing the next morning.
So many hopes and dreams depended on these results!
Still nothing.
That night in the middle of my workout session, my phone finally rang. I was annoyed that she had picked this time to finally call but I was relieved it was her, the ENT.
“I had a chances to review your daughter’s scans…It looks like your family should start learning to sign…I do not see an auditory nerve on either side.”
“Okay…” I said staring out the window at our unmanicured backyard.
The ENT continued to explain that due to the absence of Baby Girl’s auditory nerves, she was no longer a candidate for cochlear implants. Without the auditory nerves there was no path for the implants to communicate sound to her brainstem. She mentioned a new alternative option called an ABI but stated Baby Girl was probably not a candidate for that either due to her Dandy-Walker Syndrome variant.
An auditory brainstem implant (ABI) is a small device that is surgically implanted in the brain of a deaf person whose auditory nerves are lacking or damaged. The auditory nerves conduct the sound signals from the ear to the brain. The implant enables otherwise deaf people to have a sensation of hearing.
The hearing sensation is limited, but the implant recipients are relieved of total sound isolation, facilitating lip-reading.
The auditory brainstem implant consists of a small electrode applied to the brainstem, a small microphone on the outer ear, and a speech processor. The electrode stimulates vital acoustic nerves by means of electrical signals and the speech processor digitally transmits the sound signals to a decoding chip placed under the skin. A small wire connects the chip to the implanted electrode attached to the brainstem. Depending on the sounds, the electrode delivers different stimuli to the brainstem making deaf people hear a variety of sounds.
Due to the brain surgery required for the implantation and the limited effectiveness of the implant, the number of implant recipients is small.
So that was it. Our daughter was deaf and there was nothing we could do to change that.
I’m guessing you are wondering, as we were, then why did everyone think she could hear? Why did she respond to sounds that were out of her line of vision? Why did everyone report how much she loved her music? Welcome to the club! And that is why Baby Girl/Squirrel has another nickname: Alien Mystery Baby. Nothing about her seems to make sense, she leaves many of her doctors scratching their heads, and most tests leave us with more questions than answers. I’ve had doctors ask out of medical curiosity if they could follow her for their own education. I used to like to joke that someday her condition would end up in medical books bearing her name: [Baby Squirrel] Syndrome.
When I got off the phone with the ENT I expected to cry but I didn’t. As I try to remember what my immediate feelings were, my chest fills with weight. I had been trying to prepare myself for this possibility for weeks, months, but I was pissed. We were devastated. I know that to the Deaf community, that can be offensive, but Paul W. Ogden, author of The Silent Garden: Raising Your Deaf Child acknowledges that your child’s deafness is a crisis, at first.
“…a crisis is an occurrence that permanently alters our understanding of reality; frequently it is an event we have not anticipated or prepared for. Something happens that throws everything we know, feel, and understand about our lives and those around us into a new light. I don’t have to tell you that learning of your child’s deafness is this kind of experience… For the child who has been deaf from birth or shortly thereafter, nothing has altered. For you, life has changed permanently… Simply understanding that you are in the process of adjusting to a fundamental change in reality can be helpful.”
The best way I can describe it is, every time we get a new dire diagnosis for Baby Girl, I mourn the loss of the life I had envisioned for her. Starting with the first diagnosis of a cleft lip in utero, I mourned her perfect face, adorable newborn photos, happy smiles, a normal appearance that wouldn’t give kids an added reason to make fun of her. I had to exchange those images I had dreamed of for many painful surgeries, years of speech therapy, dental surgeries, multiple cosmetic surgeries, all in the hope that someday people won’t notice she was born imperfect. I have lost the life I envisioned for her countless times.
“Losses are…occurrences or events that shatter dreams that are core to a person’s existence… The initial diagnosis often marks the point when a cherished and significant deam has been shattered for the parent… The parent oftentimes does not understand that it is a dream that he has lost, and therefore he is frequently confused by the grief process that follows.”
-Kenneth L. Moses, psychologist
We didn’t want to tell anyone that our daughter was Deaf at first; we didn’t want it on social media. We called and told close family members and everyone was sad. Probably a month or more went by before we told ourselves our daughter is Deaf and that’s not going to change, so why hide it?
The whole time in the NICU, what got me through was the thought that someday she could tell me she was OK. I know that her inability to speak won’t keep her from being able to tell me that someday, but the vision was to hear her voice. Now it feels like everything is thrown up in the air. The twins are now a year and a half old and our hearing son is signing but Baby Girl shows very little interest. More recently she enjoys watching people sign the ABC’s, 1-10, and my made up “Good Night”song for her when I tuck her in at night. She likes holding hands and touching faces, but most of the time she won’t look at you when you want her to and will pull her hand away if you try to help her make sign shapes. It breaks my heart when I see other twins babbling back and forth. How much I wish that was A & A; I eagerly await the day they sign back and forth. Thinking about it just makes me more anxious about Squirrel’s lack of interest in communicating.
When we tell people she is Deaf, the usual response is something like, “really? Aww, I’m so sorry!” And we dive into our spiel about how the Deaf community doesn’t consider being Deaf a disability, how we’ve always wanted to learn sign language, how we’re excited to have a bilingual family, yadda yadda yadda. Sometimes I feel that way, but sometimes I hate it. Some people apologize for trying to talk to her verbally, don’t apologize, we still do too. Whenever there is tragedy or sadness people always try to say magical reassuring phrases. Don’t do that. But I’ll get into that in a future post. One that we get often is along the lines of future technologies, “Well in the future I’m sure they’ll have someway to make her hear.” Maybe, but most likely she wouldn’t benefit from it. She was born Deaf, she’s never heard a sound, ever. Her brain is being mapped for visual information. If she heard sound, in say 20 years, her brain wouldn’t know what the hell to do with it. She would need years of therapy to learn how to hear, what sounds mean. I hope that if that technology ever is available that by then she is so well adjusted she wouldn’t need to subject herself to the hassle.
I have so much to say here and nothing. My feelings regarding my daughter’s deafness is fluid and evolving. This part of our story has such a far way to go. Sometimes I truly am optimistic about it. This is the best time ever to be born Deaf; with so much of our communications digitalized already, job are limitless. But I’m still scared about where she will fit in in life. Deaf children are more likely to have other disabilities than the general population; however, the Deaf community has also worked very hard for generations to dispel the notion that Deafness in itself is a disability, and therefore some try to distance themselves from Deaf people with disabilities so as to not be perceived as a disabled person by association.*
♦
When Baby Girl was discharged from the NICU, she was enrolled in many state and federal funded programs due to her prematurity and health issues. Shortly after she was discharged from the PICU, the Early Start Program, in conjunction with the San Andreas Regional Center (SARC), sent interventionist to our home once a week to play with and observe and assess Baby Girl’s development.
The Early Start Program is California’s response to federal legislation ensuring that early intervention services to infants and toddlers with disabilities and their families are provided in a coordinated, family-centered system of services that are available statewide.
Once we learned she was Deaf, SARC transferred her from the county level Early Start program to our local school district with interventionist and teachers for children with hearing loss. An Individual Family Service Plan (IFSP) is created every 6 months to formulate developmental goals for Squirrel based on her own abilities. Now once a week her teacher/interventionist comes to “play” with her and track her development. And every other week her awesome ASL teacher comes and works with all of us. She shared with me that she gets really excited when a new Deaf child enters their program, but has to remind herself the parents might not feel the same way.
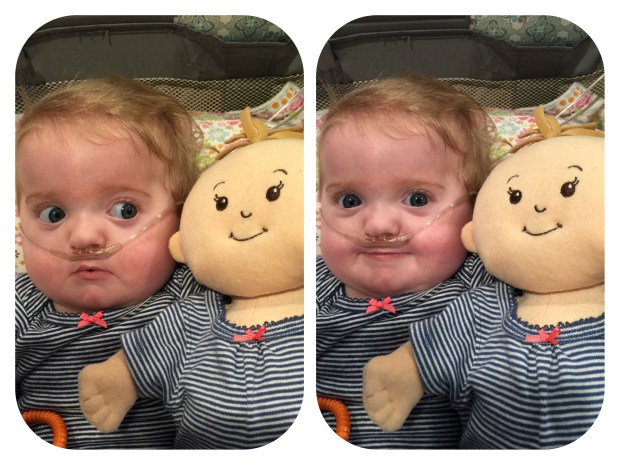
Baby Squirrel at 9 Months Old
It’s not all bad. It is fun learning ASL, I just wish it wasn’t because we HAVE to. And it’s helpful having Baby Boy be able to tell us what he wants since his verbal vocabulary is still small. It’s just one more thing on top of the mountain of other things. I am relieved she’ll never have to endure those school bus hearing tests though. From unrelated causes, I have poor hearing and the school bus tests were always humiliating for me when I was the last student let off the bus. There are definitely pros and cons to Squirrel’s deafness.
- Pros
- She can sleep through anything
- We don’t have to watch what we say around her – For example…
- We can mute Caillou
- Our protective dogs don’t wake her when people fail to read our “No Solicitors” sign
- She could get a service dog someday!
- Cons
- We can’t get her attention if she can’t see us
- We can’t startle her out of a bad behavior by yelling
- You can’t communicate while doing other tasks with your hands
- She won’t be properly embarrassed by our “80s on 8” renditions
- She runs the risk of not overhearing enough dysfunction to be funny
Our house is covered in Sign labels.



Aside from my friend’s stepdad in elementary school, my daughter was the only other Deaf person I had ever met. Watching my friend sign with her family had left an impression on me, and ever since I had always wanted to learn sign language. In college I tried to take American Sign Language but I couldn’t register because I was not a Special Education major.
Over the past year we have tried multiple avenues to learn sign language. We had to first decide whether to learn American Sign Language (ASL) or Signed Exact English (SEE). ASL is a fully formed true language with its own grammar and syntax, where SEE is English with a sign for every word. We ultimately decided that it was most important to give Squirrel a basis in real language and chose to learn ASL. My older sisters and one of my nephews are learning SEE at our local school for the Deaf and Hard of Hearing. My nephew tells me everytime I see him that he hopes Baby Girl learns to sign and her oxygen and feeding tube goes away so she can have a normal life. *tear* He’s 8 and he told me he was so sad when he found out she couldn’t hear. Me too, Buddy.
My husband and I tried online tutors, and watching DVDs, but being in the house with the kids is too much distraction. This spring semester I began taking an ASL course at our community college. Three hours every Monday night. It’s already been so helpful to get out of the house and immerse myself in the class without interruption. My professor is Deaf and speaking is forbidden in class. I was surprised by how much I already know.
I didn’t actually get into the class at first. I was 6th out of 13 on the waitlist, and she only ended up taking the first four. Since it was the first day of class most communication was written on the chalkboard. I got up and wrote asking if I could audit the class, just sit in the back and watch. She signed no, there was no room, nothing she could do. So I put down the chalk and I signed, “My daughter is Deaf.” She told me to sit down and handed me an add code at the end of class! The Deaf culture is collective, they take care of their community and share any information they can to help Deaf people communicate and interact with the hearing world around them. By helping me she’s helping my daughter.
♦
I’m not one to believe in fate or really anything divine, but something along the way happened that I truly am thankful for, and kind of in awe of how perfectly these people came into our life. While I was pregnant our hospital enrolled us in a prenatal group called “Centering.” It was awkward at first but we were all due around the same time so slowly we bonded over common pregnancy symptoms, and the dads bonded over how crazy all the moms were. Just kidding, they bounded over sports and other off topic subjects. There was even another couple having twins.
I was the first one to pop. But exactly a week later, while we were visiting our babies in the NICU, we ran into a couple of familiar faces. The other couple with twins delivered their boys at 32 weeks and they were also in the NICU. We got closer over time, mostly from seeing each other in the NICU all the time, and going through a similarly difficult situation. It was nice to have people we knew there.
After all the Centering group babies were born everyone met back up for a reunion, Baby Boy was home by then. We exchanged information and started meeting once a month for playdates. These families have turned into an extended family to us and our kids: aunties, uncles, best-friends growing up together since before they were born.
The coincidently perfect part is, the mother of the twin boys has many Deaf family members and was raised with ASL as her primary language. You know who you are, and it still makes my eyes misty to remember the first time we brought Baby Squirrel to your house, and as we were leaving you knelt down infront of her car seat and signed to her. I have no idea what you said, nor is that important. But I don’t think you have any idea what that meant to me. Thank you.
♦
This chapter is open ended – this part of our journey is still just beginning. Stay tuned for updates. Including upcoming posts about more things for people to stare at, and getting a genetic diagnosis!!!!!!!

*If you have a child recently diagnosed with hearing loss, I highly recommend reading The Silent Garden: Raising Your Deaf Child, by Paul W. Ogden.































 All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.
All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.