Post Traumatic Postpartum Neonatal Intensive Care Unit Depression Stress Disorder
OK, maybe I made that up. But I wasn’t just effected by the twins emergency 9 week early arrival, or their 4.5 months in the NICU, or the wild hormonal changes swirling through my brain and body after pregnancy; they all played a nasty game together.
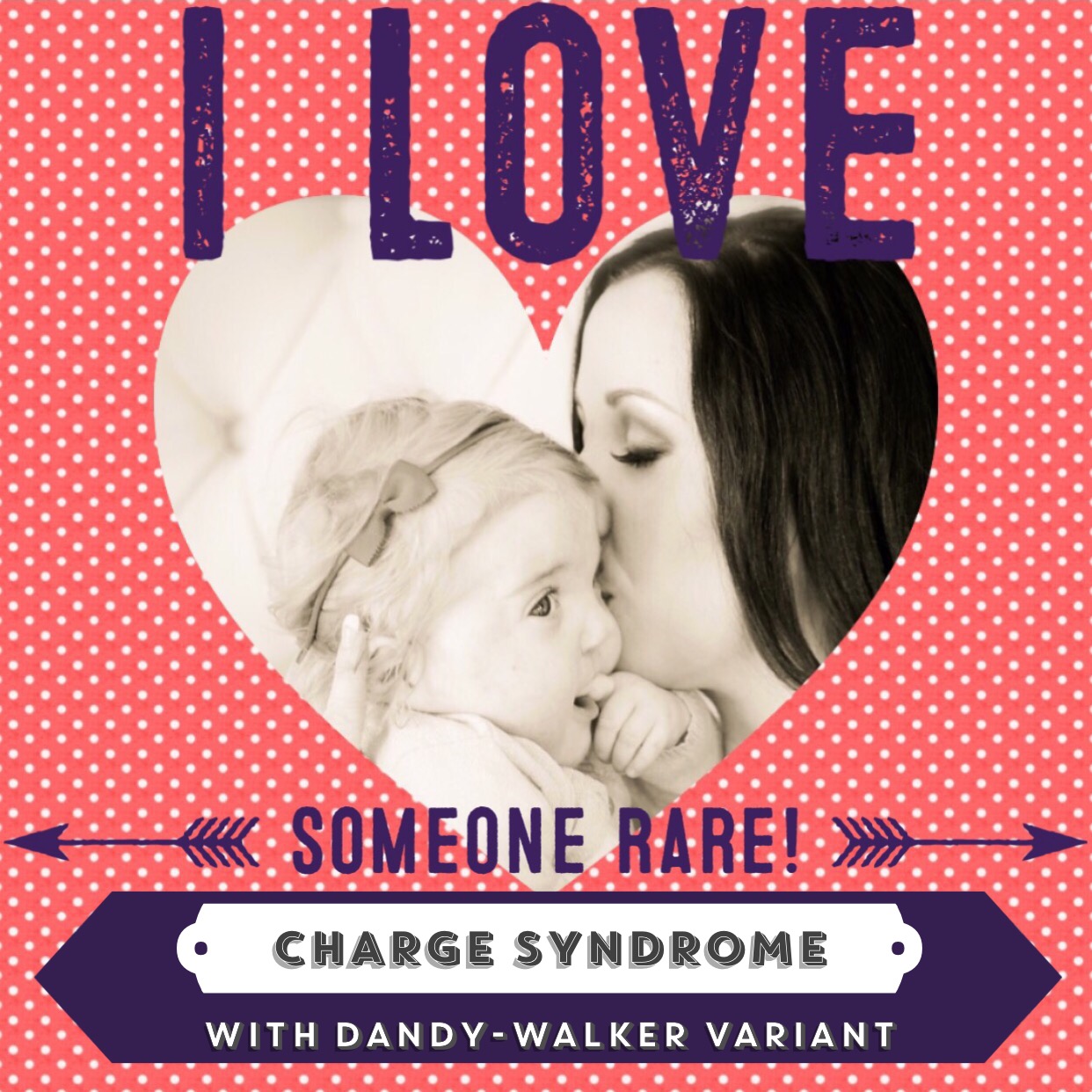
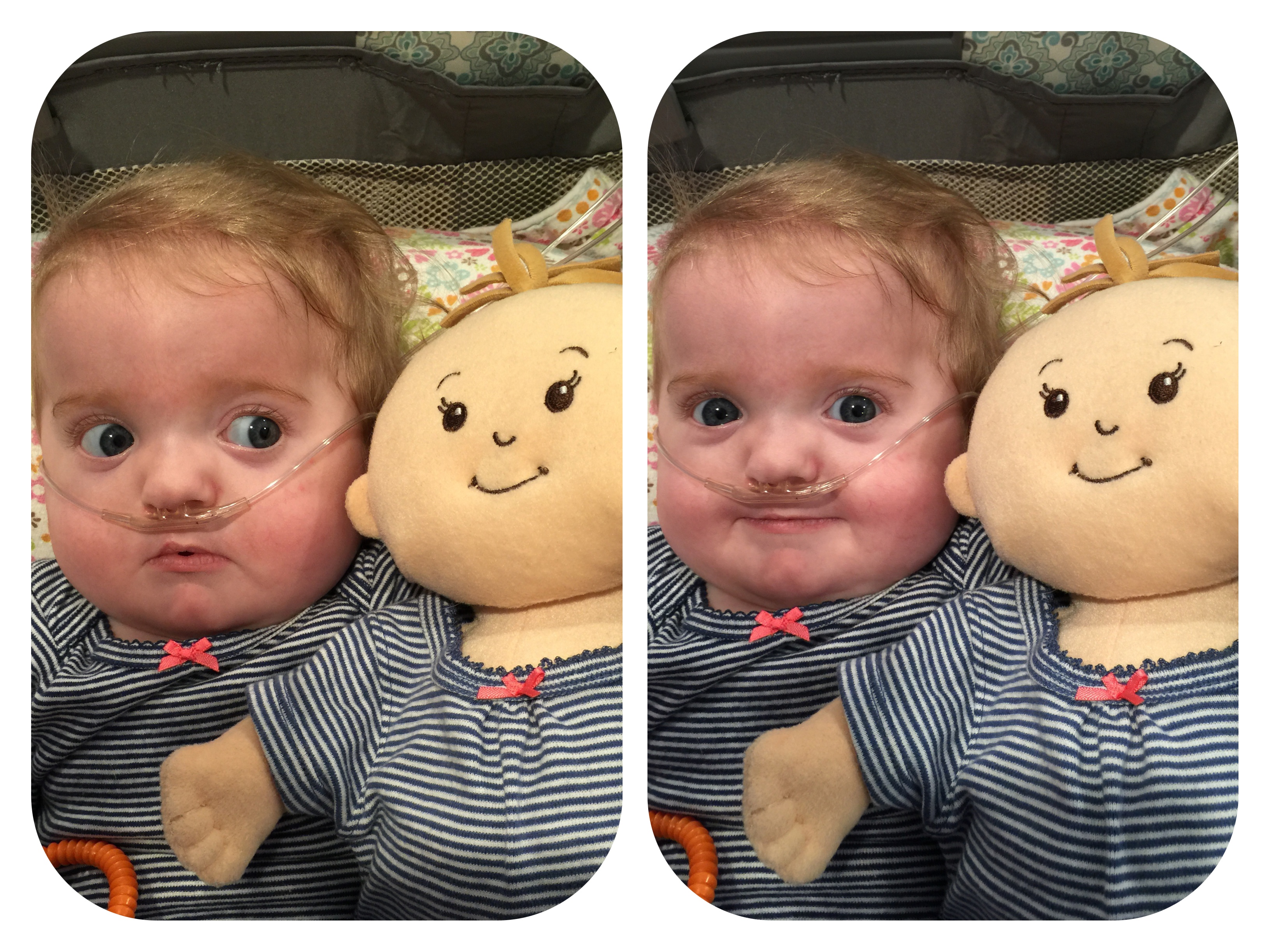
Few people know many details about our 133 day stay in the NICU because it got to a point where it was too painful to continually tell people our daughter wasn’t any better, or she was continually getting worse, or she had received another dire diagnosis. We appreciated everyone caring enough to ask but they most likely received a lie in response. “She’s doing alright,” “she’s still technically premature so she still has a long way to go,” “her lungs just need to get stronger and she’ll be home,” “eh, she’s getting there.” I rarely to never shared photos of our daughter during this time because, quite frankly, she looked like shit. I’ll do my best to not make this post horribly depressing but the truth is I am still profoundly effected by our experiences over the last year and a half. And I still struggle with depression every single day.
When the twins were born on September 3rd, 2014, 9 weeks early by emergency C-section, I didn’t get to see them for the first time till the next day. They were still an abstract idea to me; you know you’re pregnant but you’ve never seen them outside your body before so you don’t really know who you are missing. I even still felt their fantom kicks. I was in so much pain I was switched to Percocet and kept in a sleepy haze. Most mothers will probably disagree but I loved having a catheter in because it meant I didn’t have to get out of bed. (I had to pee and then I didn’t anymore. It was fantastic.) My husband had seen our children when he escorted them to the NICU where he fought with the nurses and doctors to get them placed next to each other rather than in two completely separate areas.
While I was in recovery he spent time with the twins and took pictures but he refused to show me until I was able to see them in person. All I knew for almost 24 hours was that my son had dark hair like his daddy and my daughter had strawberry blonde hair like me. And that her face was completely open on her right side due to her cleft lip and palate. We knew she would have the clefts before she was born but we were never able to see if her lip was open all the way up through her nose or not. Every 2-4 weeks I was given a 3D ultrasound to try to see her face (moms of typical children are probably envious of that), but she always either had her face up against the membrane that separated her from her brother, which made the image look like she had a veil over her face, or her brother’s butt was in the way.
The day after their birth it was my mission to get out of bed and into the wheelchair so I could go see my babies. Holy fuck! You really don’t realize how every move you make uses your core until your core has been sliced open and stapled back together. It took two people and a lot of crying but I made it into the wheelchair and over to the NICU. We had always known that with twins it was almost a guarantee that one or both would spend at least some time in the NICU; however, I was extremely naive of how that would actually effect us.
Their first 4 days in the NICU are kind of a blur for me. I was on heavy painkillers and spent my time there fighting the nods while peering through the little door/windows in the side of their isolettes, cupping Baby Girl’s head in my hands, or sitting next to Baby Boy’s isolette holding his tiny fingers sobbing because every breath he took looked like his ribs collapsed to his spine. It would be 5 days before I was able to hold my son for the first time, and 10 days before I could hold my daughter. You may notice I talk about my son much less than I do my daughter. Once my son’s lungs opened up he was able to breathe on his own. For the rest of his time in the NICU as long as we let him sleep on his tummy he was happy.
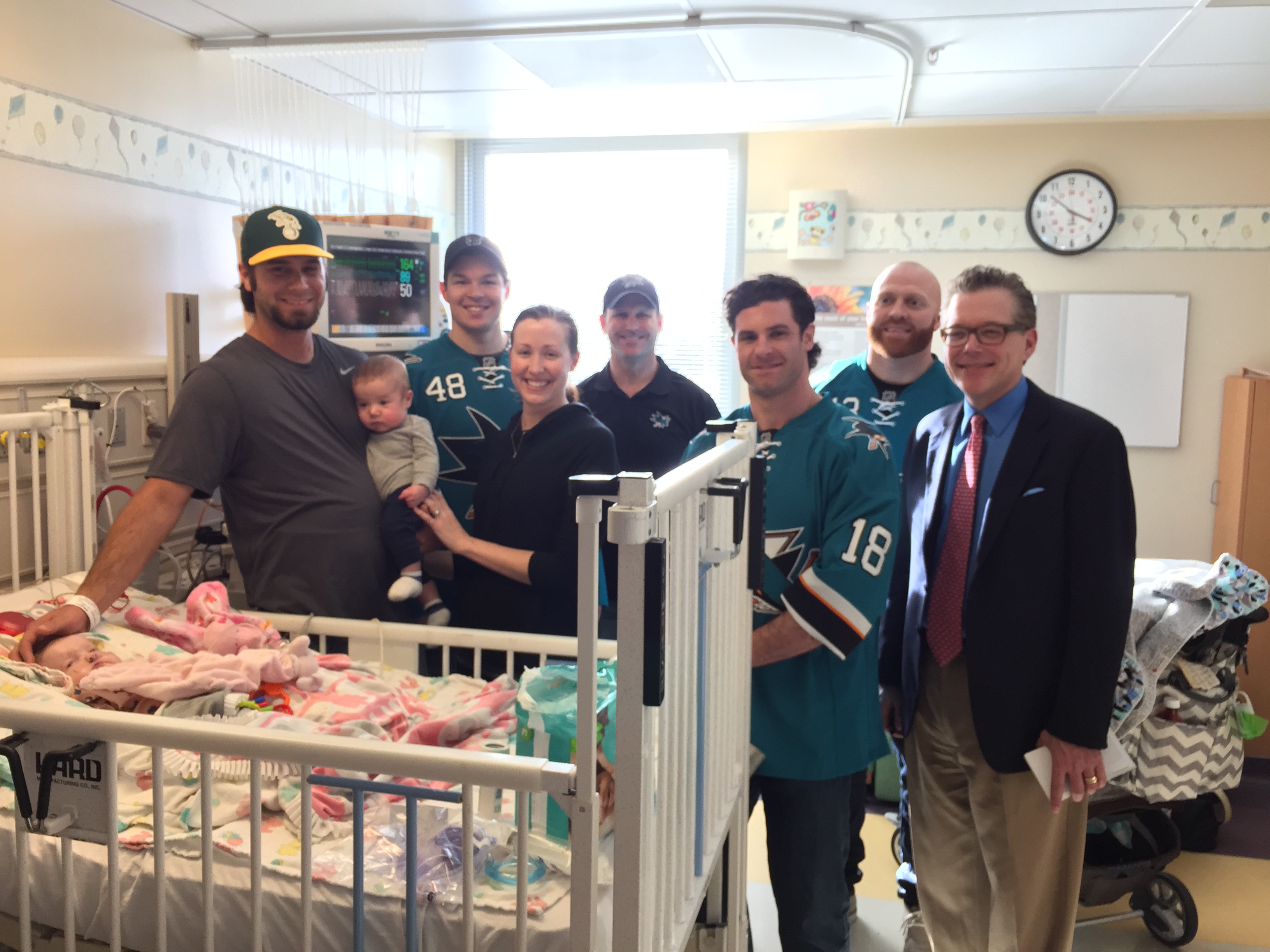
Because they were 9 weeks premature the doctors expected them to remain in the NICU for 4-6 weeks. Because we knew we were in for the long haul we showered the NICU nurses with Starbucks coffee and giant gourmet cake pops made by a close friend who was a pastry chef. My charming husband made sure all the nurses and doctors knew us all by name so they would consciously, or at least subconsciously, take the best care of our babies when we couldn’t be there.

The massive sunflowers hide that these cake pops were huge!
I remained in the hospital for 5 days, before being discharged. I got my wheelchair ride out but my arms were empty. I sobbed all the way home leaving our babies behind. I don’t think that crying ever really stopped after that. I woke up crying, I pumped crying, I fell asleep crying. I relied on my husband for everything. Physical support, emotional support, and he carried it all like the Titan Atlas.
Pumping, pumping, pumping, pumping, pumping, pumping, pumping, pumping. Fuuucckkkk pumping. Pumping 8-12 times a day, every 2 hours, roughly a 40 minute routine. Do the math with me here, that’s nearly a minimum of 6 hours a day. But not just during the day – around the clock. And the 2 hours starts when you start pumping, so really you only have an hour and change between pumps. I killed myself for that milk and it always made me feel like a complete failure. I could never produce enough for both. When I would take that sweet liquid gold into the NICU the nurse taking it would always say, “thats all? Are you pumping at least 8 times a day?” I wanted to be a breastfeeding mother, my goal was at least a year. I knew it would be hard but it’s fucking hard! I tried everything. Supplements, massage, “Power Pumping”, I was spending that 6+ hours a day online researching how to up my supply. My daughter would never be able to breastfeed due to her cleft lip & palate, and my son would end up taking 8 months to figure out milk came out of those things! 8 months! ANYONE that says “don’t cry over spilled milk” has never been a lactating mother!
For the first week home, we would get up and go to the NICU, spend all day there and then come home and do it all over again the next day. The NICU at our hospital was a level III NICU but the babies did not have private rooms. There were 4 main rooms called Pods: Pod A, B, C, and D, and each pod had 6 isolettes/cribs. You could pull a curtain for “privacy.” The nurses had shift change every day at 7am, 11am, 3pm, 7pm, and 11pm. At those times all parents had to leave the NICU for 30 minutes before they could come back in; you couldn’t stay with your child around the clock.
After a week I was healed well enough to care for myself and get around on my own. My husband returned to work so he could save his paternity leave for when the twins came home. I was so scared to be alone. I had become completely dependent on him. I was constantly crying and sad and he was constantly reassuring me and trying to ease my fears. All the stress surrounding babies that could have torn us apart had brought us exponentially closer.
I delved into a routine in an attempt to keep my sanity. Every morning when my husband left for work I would get up, pump, then head to the hospital to deliver milk. I would stay for 9am rounds where the doctors and staff would come around and talk about all the scary stuff wrong with our children, particularly our daughter. Blood clots in the brain, hydrocephalus, inability to feed, failure to thrive, heart murmurs. I would stay till about 11:30am then head home. I would drive back to the hospital again at 4:30pm to meet my husband and we would stay till shift change at 7pm then head home and start dinner.
During the 2nd week our daughter stabilized enough to be held. I was terrified. She had so many tubes and wires and cords attached to her and she was just so tiny. Looking back at photos I can now see how mottled her skin was and why the doctors were so concerned about her coloring. Shortly after she was put in my arms she refluxed and threw up all over me. The bile itself I didn’t mind. It was the vision of it coming out of her mouth and nose because of her clefts. It gushed out of her entire face and then she would choke and turn blue and the monitors would start screaming. Those goddamn monitors. Constantly going off. Today I can read those monitors upside down and backwards, but then I didn’t know what they meant and the sound always scared the hell out of me. Every time one would go off I would jump. And because the pod was open I could hear all the other babies monitors, and sometimes I couldn’t discern immediately if something was wrong with my babies or someone else’s. Most premature babies have a feeding tube in their nose down to their stomaches. When my daughter’s reflux could not be managed and continued to be threatening her doctors opted to move her feeding tube past her stomach and into her intestine with an x-ray guided weighted tube with the goal of reducing the amount of content in her stomach. Like most things with our daughter we would learn, it only helped a little. I just kept telling myself that someday I’ll get to hear her little voice tell me she’s OK. I’ll explain in a later post why that will never happen.
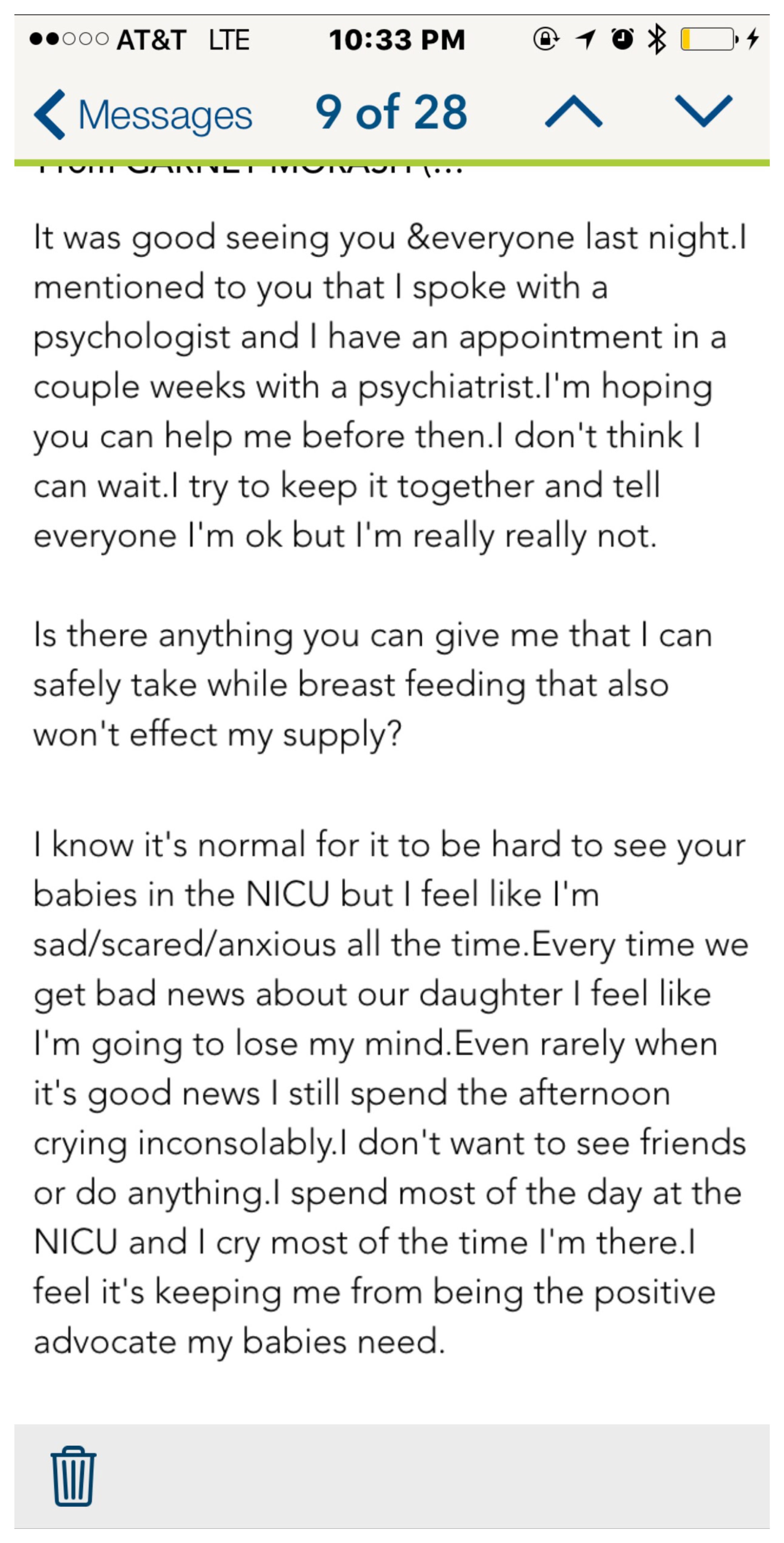
One doctor noticed that I would always cry when we spoke after rounds, or any time for that matter. She always asked if I was OK and offered to have a social worker come talk with me. I always said I was fine, I was just scared, and I didn’t want to talk. After a male doctor (let’s call him Dr. K) bluntly told us our daughter had a hole in her heart and would probably require open heart surgery, my husband had privately requested that the doctors speak with more tact around me. However, one day we were told Baby Girl had fluid pooling around her brain causing added pressure. I remember our primary nurse hugging me for the first time and that I felt things must be much worse than they are letting on in front of me. I asked to speak to the doctor that always checked on me and told her I was ready to talk to someone. I was set up with appointments to speak with a therapist and a psychiatrist. I didn’t want medication but I was instructed to keep the appointment anyhow. I don’t even like taking Motrin for headaches till I’ve at least tried to drink it away with water.
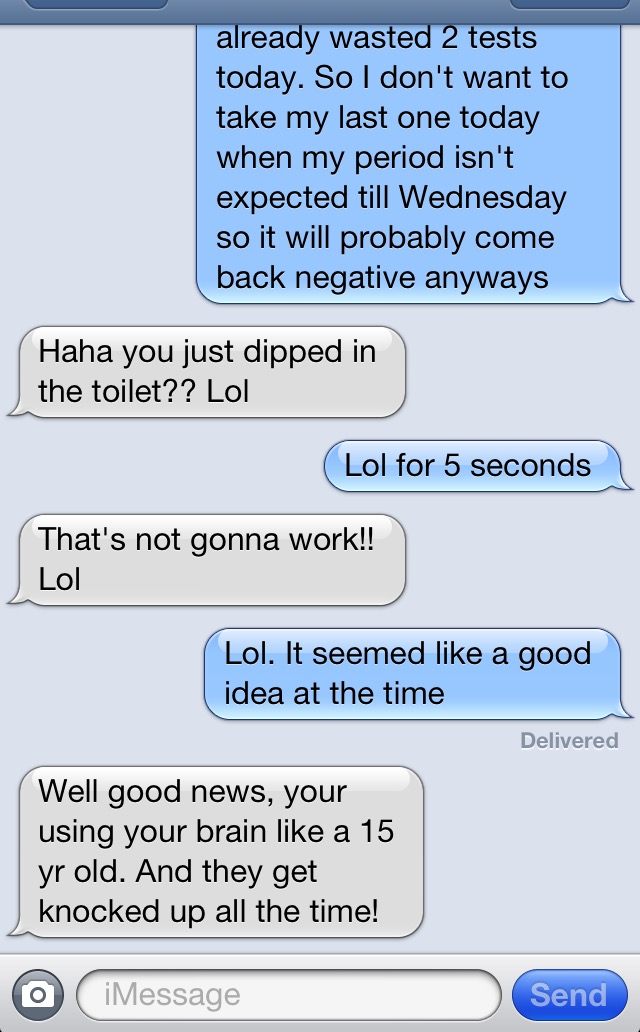
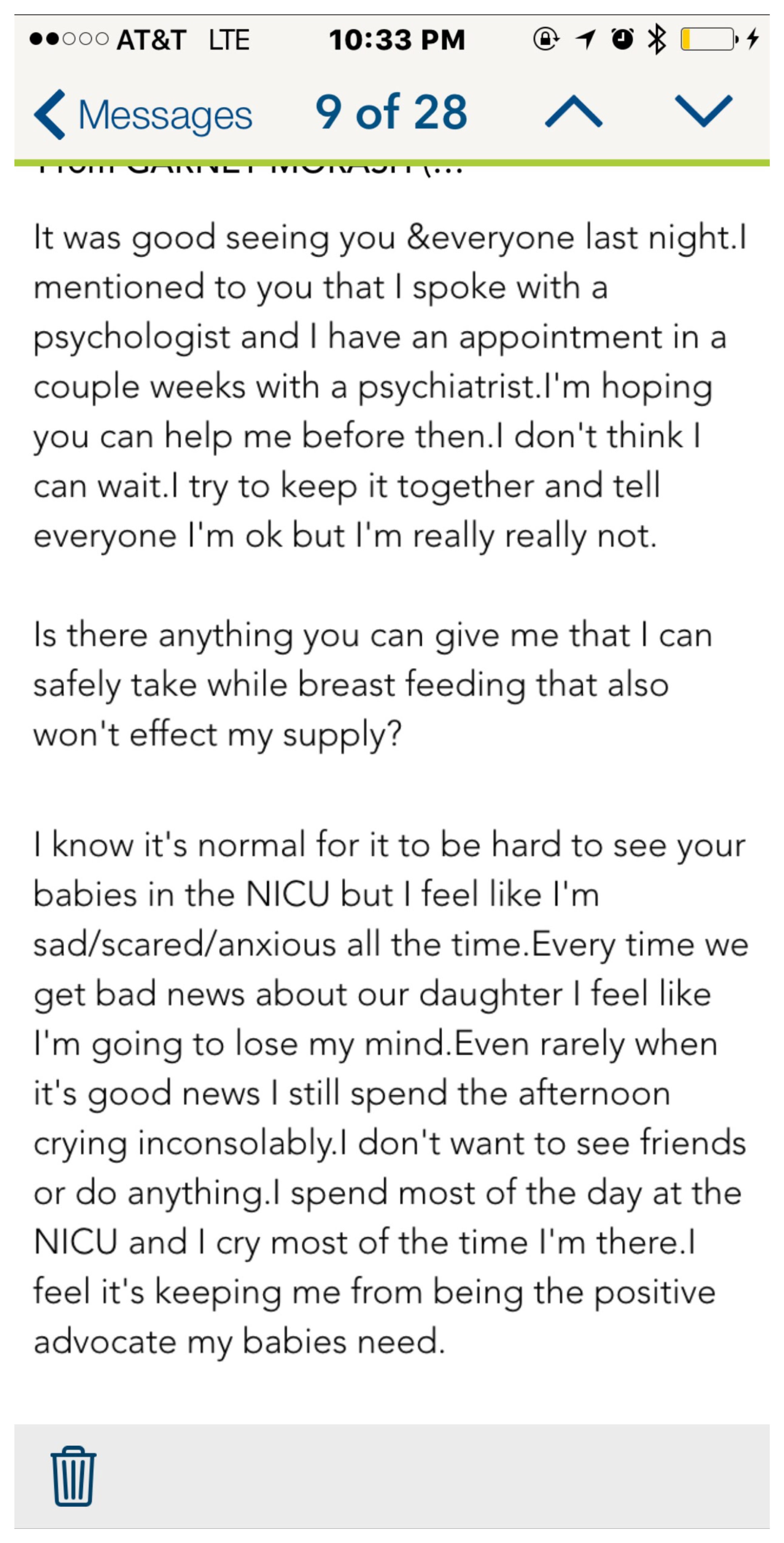
Three weeks doesn’t sound like a long time now but by their third week I was losing it. I wasn’t sure if my daughter was going to ever leave the hospital alive, I was only sleeping and hour or 2 tops at a time, I felt nauseous all the time, postpartum morning sickness as I began to call it, and mentally I was a complete wreck. Imagine every negative emotion coursing through you all at the same time constantly for over 20 days straight. Sadness, fear, anxiety, worry, exhaustion, disappointment, regret, loss, inadequacy. And I don’t mean like I was bummed out or feeling blue. My chest ached with deep terrifying sadness and fear. I felt completely useless to my children. I regretted having them at all. I showed up to the NICU multiple times a day but I didn’t want to be there. I pumped nonstop for them but I fucking hated myself when 30 minutes later I only had an ounce or two to take to them. When doctors would talk to me I could only nod and fight back the tears, I couldn’t contribute to the conversation or to the care of my children. Every time those motherfucking monitors would go off my heart would race and I would go into fight or flight mode. And one day I snapped. Both of my children’s monitors kept going off, back and forth, loud piercing beeps in the mandated quiet of the NICU. I wanted to get up and run out of there but instead I grabbed my phone and penned a desperate email to my OB.
My desperate plea to my OB
My OB headed a special prenatal group we attended and we got to know each other very well, much more so than just occasional check ups. So she wasn’t just passing out pills just because I asked. She prescribed me Zoloft and I picked it up that night. Zoloft is in no way a quick fix. In fact it makes things worse before they ever get better.
I had agreed with my therapist that I would attend a Postpartum Depression support group. I didn’t think it was the right fit for me but I agreed to check it out. **In advance, mothers, please forgive me for my thoughts I am about to share from this time. I know any mother can experience PPD, no extraneous circumstances necessary.** The group consisted of about 10 women, all but myself and one other mother had their babies there with them, all singletons under 6 months. We moved clockwise around the group introducing ourselves and sharing what we were struggling with. The first mom was beautiful and put together, hair done, light makeup, well dressed. She talked about how she had got to go out with her girlfriends over the weekend and how nice it was but how the baby woke up at 2am that night wanting to be feed and that was stressful for her. The next mom shared that she couldn’t get any friends or family to come over and help give her a break from her baby, her son nursed while she spoke. Another shared that her son was born 11 days early but did not have to spend any time in the NICU and she was sad all the time, and that her husband had earlier that day watched their son so she could get out and get a pedicure. I wanted to scream at these pathetic women, “You have your healthy child attached to your tit right now, what the fuck are you crying about?! I would give ANYTHING to be in your shoes. My children are fighting a possibly losing battle for their lives right now!” I didn’t of course. Instead when it was my turn I started hyperventilating/ugly-crying halfway through my name. I bawled out my situation and vowed to myself I wasn’t coming back. The poor girl after me said she had the “postpartum blues.”
The first 10-14 days on Zoloft were the worst. I didn’t think it was possible but everything negative intensified, even the nausea. After about two weeks everything finally began to improve. I met with my psychiatrist and we increased my dose over time to an effective level. I am not ashamed to admit that I am medicated. It is the best thing I have ever done for my kids and marriage. Once the medication took effect I could control my emotions. I could hold a productive conversation with the doctors and discuss my children’s care without crying. I could think reasonably and logically. And best of all I began to see the positive sides of everything; I saw everything as blessings in disguise. Every time my husband and I had received bad news, we made “positive positive positive” our mantra, and now I could really live it. I wasn’t manic by any means, I still felt sadness and anxiety but at a manageable level. My husband recently told me in the past he thought people that needed antidepressants were weak but after our experience he saw that some people really do need them and they can help immensely.
During those long two weeks, after 31 days in the NICU, our son came home. He was technically still only 35 weeks and tiny, just over 6 pounds. Leaving the hospital with our son was even harder than the day I was discharged after their birth. I felt like we were abandoning Baby Squirrel. She was still so little and sick and we were going home and being happy with our healthy baby boy. Every joy felt like a betrayal to her. It was like living in two different worlds. In the NICU everything was solemn, but at home we were making memories and becoming a family. Our son was growing and developing and thriving and the gap between him and his sister was growing larger.

Baby Boy’s Homecoming
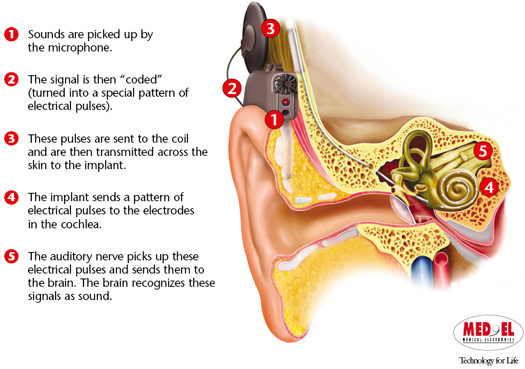
When Baby Girl was nearly 40 weeks old they moved her out of the typical isolette and into a crib. We brought every stimulus we had. A mobile with colorful birds for her to look at and reach for, pictures of us and high contrast images to tape to the sides, a vibrating chair, and an iPod and speaker full of calm upbeat and relaxing music. She loved her music. Her nurses kept it on for her quietly 24/7. Every day the nurses would tell us how much they loved all the Beyonce, I accidentally put 3 copies of “Halo” in her mix. And they always commented on how much Baby Girl loved her music, how she perked up when it came on. Six months later on my 30th birthday we would learn how ironic their comments were.

 All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.
All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.
I think I shut down. I don’t remember much after hearing that. I can’t remember if I was just numb from the daily stream of bad news or if I was protecting myself for her possible demise. I think that was the universal tipping point; the universe decided we’d earned a miracle. During a follow up echo a couple days later the cardiologist found her VSD, the large hole in her heart that Dr. K said would require open heart surgery, and that the cardiologist later refuted but said would take years to close, had closed seemingly over night. Before telling us the cardiologist had other cardiologist confirm it because he did not believe what he was seeing. Later that day at rounds, Dr. K said, “I’m not supposed to say this but she must have a lot of people praying for her.”
We rode that high as long as we could. But Baby Girl’s reflux was not improving. Dr. K proposed giving her a g-tube and tracheotomy. We refused. I adamantly did not want my daughter to have a g-tube. The thought of them cutting open her perfect, soft, smooth belly skin was unbearable. Just the sheer thought of it made my eyes well up and spill over.
In early/mid November all the nurses went on strike. Due to the delicate nature of the NICU, the nurses brought in travel nurses and quietly warned all the parents so they could prepare. For 48 hours my husband stayed with her to make sure there were no set backs due to nurses that were inexperienced with her very particular care instructions. For 48 hours he stayed with her, sleeping in a straight backed chair and leaving only at shift changes. This ended up being a blessing in disguise as the travel nurse that had our daughter taught us how to take care of our daughter, and further more, she let us. By the end of the two days we felt much more comfortable with her routine care.
The discussion over a g-tube and trach continued for days before my husband made it very clear that the word “tracheotomy” was not to be uttered ever again unless they could guarantee that it would fix all her breathing issues and allow for her to come home, they couldn’t. However, after much back and forth we consented to the g-tube. They assured me that it was just a tiny hole and once she learned how to eat normally they would take the g-tube out and there would only be a small scar. The hope was that if we could get the feeding tube out of her nose and throat she wouldn’t gag and reflux anymore. Surgery day came and we felt reassured that the performing surgeon had actually performed a major chest surgery on my husband nearly 15 years earlier. The surgery was quicker than expected and Baby Girl’s pain was manageable.

Baby Girl’s first g-tube
Unfortunately, the g-tube didn’t stop the reflux. She needed a pediatric Ear, Nose, & Throat specialist but the closest one was nearly an hour away in Oakland, CA. She was transferred via ambulance with her daddy in toe for what was intended to only be a couple days. Once there and settled in the ENT scoped her nose and throat and found she had a hiatal hernia, the upper part of her stomach was pushing up through the diaphragm and into her chest region. She would need a Nissen fundoplication surgery to repair it.
Nissen fundoplication, also known as laparoscopic fundoplication, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD it is usually performed when medical therapy has failed, but with paraesophageal hiatus hernia, it is the first-line procedure.
-good ol’ Wikipedia
The surgery would be done with scopes through tiny holes in her belly and down her esophagus and was expected to take only a couple hours tops. I told my husband to call and update me the second she got out of surgery since he was there with her and I was at home with our son. When you have a newborn/preemie at home time ceases to follow its typical trajectory and I noticed 4 or 5 hours had passed and I still hadn’t heard from my husband. I called him and jokingly chastised him for not calling me when she got out of surgery and asked how she was doing. He didn’t know. She was still in surgery and no one was telling him anything. He even went and looked for her back in the NICU thinking maybe they had taken her straight back up there and forgot to come talk to him.
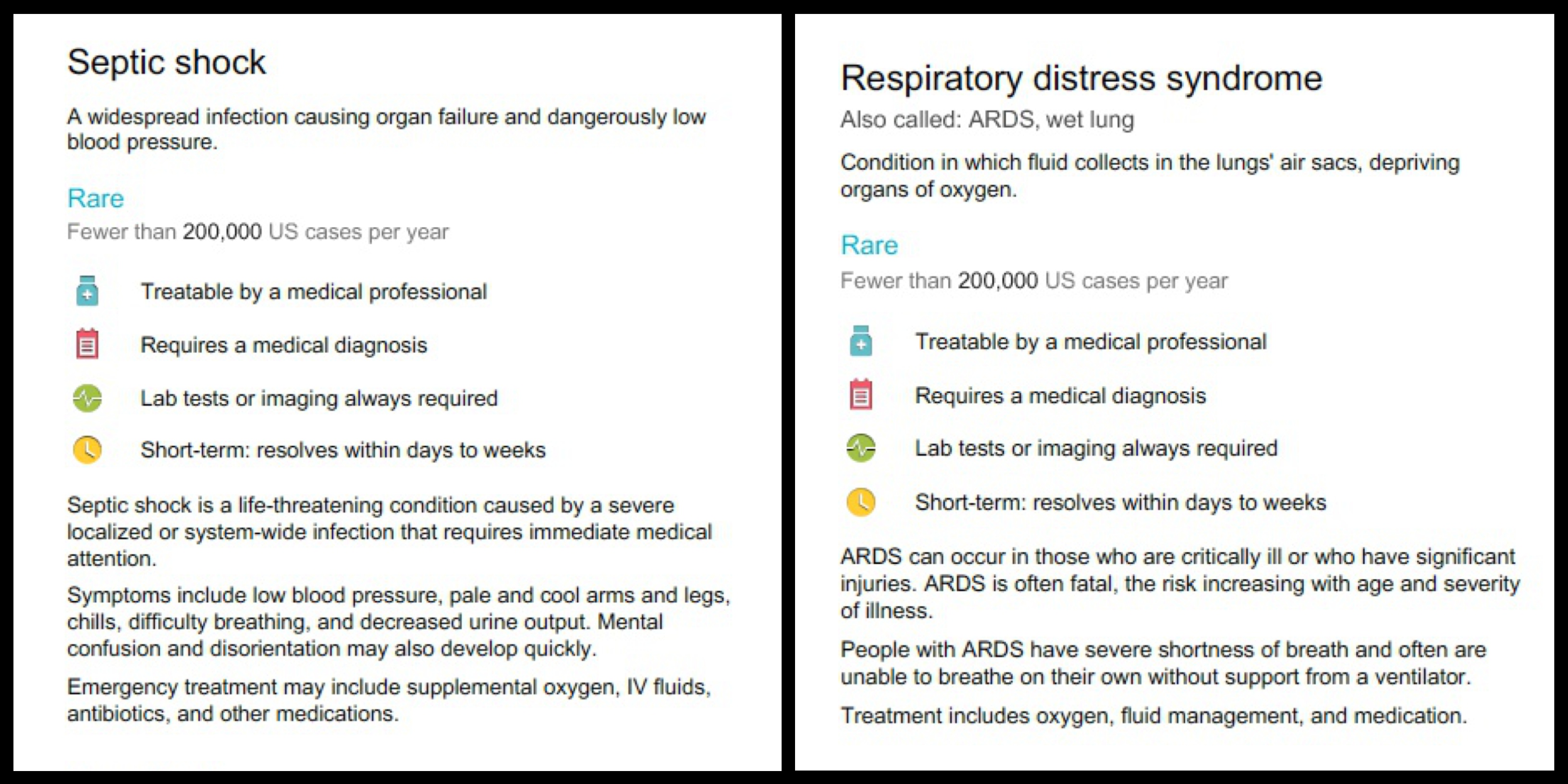
After 7+ hours a doctor emerged to inform my husband that her Nissen was successful, but they had found that during her previous surgery to place her g-tube the surgeons had perforated her bowel and colon causing fluid to leach into her abdomen. To repair the damage and save her from developing sepsis they had to make a large incision across her stomach above her belly button and remove the damaged sections of her bowels and colon. So much for worrying about a tiny g-tube scar, she would now have a scar to rival my c-section incision.

Bloated after over 7 hours of surgery, sporting a fancy new g-tube button

Abdominal scars
It took her three weeks before she was stable enough to be transferred back to our home hospital. Her daddy stayed with her the whole time and made it back just in time for Christmas.
The Nissen had greatly improved her reflux, as long as she wasn’t fed too quickly, but she still wasn’t tolerating any food by mouth without inhaling it into her lungs. For the next month it was a continual boomerang of oxygen support. They asked for our consent to start her on a stronger diuretic, one they had warned us about when she was born, Lasix. Lasix is a very effective diuretic but also strips the body of electrolytes and potassium so she would need routine blood work to prevent damage to her heart and kidneys. After only one dose and she was able to come off oxygen. Again she completely surprised the doctors. She still had pulmonary hypertension and chronic lung disease so after about a week she needed to be put back on oxygen but only a very small dose. We got to the NICU one day to find an almighty Discharge Checklist next to her crib. We were so excited! Her discharge was finally looming in the near future. We were ready for the challenge in front of us because at least we wouldn’t have to come to the hospital every. single. day.
In true to Baby Squirrel form, a discharge date would be set and then moved back. A date would be set and then she would randomly experience apnea over night while in the care of a nurse that wasn’t familiar with her, thus restarting the 5 day waiting period before she could go home. Then she had to pass a car seat test proving she could make the 20 minute drive home safely. Again, against our strict orders, a night nurse performed the test and she failed due to the pads being in the incorrect position causing her oxygenation level to drop. This presented a huge setback. Now the only way they would let her go home was in a “car bed” which would need to be special ordered. Amazon to the rescue!! This thing felt like a freaking death trap the way it precariously attached in my car but on January 14th, 2015 I got my final wheelchair ride.

The scariest wheelchair ride of my life!

Saying goodbye to our children’s NICU aunties and Grandma, their primary nurse, was extremely bittersweet. They had been our family for nearly 5 months. They were the only people in the entire world that knew exactly what we were experiencing every day. On Baby Girl’s final day I left this letter to her team:
Dear [primary nurses’ names] and ALL the nurses that care for, talked to, played with, held, comforted, and loved our daughter:
We can never repay you or thank you enough for the gift you have given us. Thank you for being [Baby Girl’s] mothers while I could not.
We are so overwhelmed with excitement to finally have our family whole and be able to bond with both our children. You have been our family for the last 4 months. You have witnessed the hardest days of our lives. Your kind hearts comforted us when [Baby Girl’s] mounting prognosis felt dire. You are forever in our hearts every time we look at our beautiful children who have taught us how precious and fragile life can be. I cannot come up with the right words to truly express our gratitude.
We will truly miss all their aunties & grandmas.

Saying goodbyes
Leaving the NICU my sister took one last picture of Baby Girl’s empty pod…
Still to this day I cannot articulate how morose this photograph makes me feel.

Baby Squirrel’s Homecoming
In conclusion, over a year later, some days I feel like I am ready to get off Zoloft, I have even reduced my dose a bit. But then there are times that I’m not sure I could handle caring for all my daughters special needs without it. When Baby Squirrel is happy and smiles or laughs my heart swells with joy unlike anything I’ve ever experienced, it’s so amazing and wonderful and I don’t know how I could love someone so much. But when she is irritable and sick and crying for hours/days on end or shitting and vomiting nonstop I want to shoot myself in the face (metaphorically speaking, I promise.) I don’t want to stay on medication forever but it’s still something I’m struggling with daily. Currently my daughter is in the middle of another asthma episode. She wakes up multiple times a night crying inconsolably, coughing and desaturating thus requiring additional oxygen till she can recover. She doesn’t have a typical cry, due to multiple factors it’s quieter and courser but it burrows into your brain and eats your goddamn soul. Along with her pulse oximeter and feeding pump we now have to haul her suction machine upstairs every night and back down again the next day. She requires 30 minutes of multiple nebulizers 4 times a day followed by CPT (chest physical therapy.) I do all this while also caring for her twin brother, who is now running all over the place and getting into everything, and while trying to keep the house in relative order. I can’t take her anywhere for fear of her catching another cold and landing back in the hospital again (those exciting tales to follow in later installments.) Which leave me feeling full of regret that my son is missing out on countless experiences because of his sister. This was not intended to be a pity-party or a sob story but rather to paint a picture of my daily reality and why I don’t feel ready to get off my mediation at this time. Maybe I’m weak but our daily life is entirely too overwhelming without a little chemical help. And on the worst of days bottle-o-wine help. 😉
I know this was an exceptionally long post; thanks for sticking with me as I try to bring our story up to speed. Below are more mostly unshared photos from our time in the NICU. Coming up next: the twins at home, Baby Squirrel’s long awaited cleft lip repair, and her very real, very close call with death. 
This slideshow requires JavaScript.














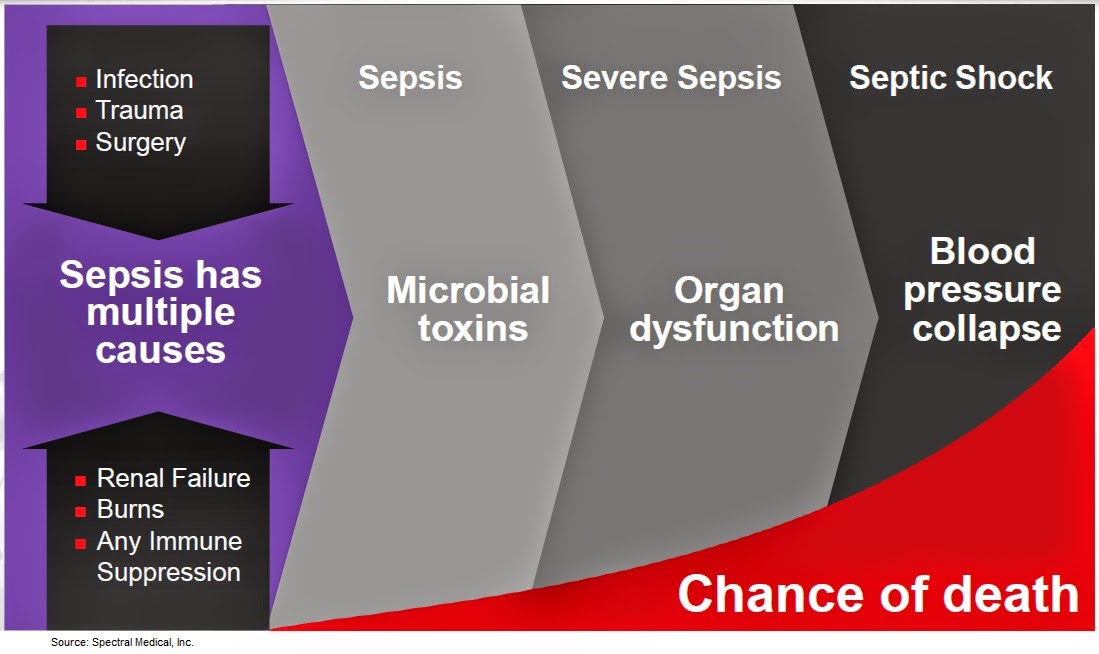






















































 All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.
All progress with Baby Girl was painstakingly slow. Even with the feeding tube down in her intestine she was still refluxing and aspirating. She was always going up and down on oxygen support. Due to her prematurity she has chronic lung disease, her lungs are riddled with scar tissue and continually fill with fluid, requiring more and more diuretics to dry them out. She had regular echocardiograms to watch how her heart and lungs played together. (My heart is currently pounding in my chest as I try to formulate this next sentence…) At two months old she was diagnosed with Congestive Heart Failure. Without knowing what that meant, it sounded like a death sentence, right?! “Heart Failure.” That super vital organ that keeps you alive, hers was failing.